Configure Eligibility Calculations and Reviews
After completing this unit, you’ll be able to:
- Describe how automatic eligibility calculation works.
- Explain how a guided flow accelerates benefit reviews.
- Summarize how caseworkers handle changes of circumstances.
Applicant Eligibility
Determining applicant eligibility is an important, yet often tricky aspect of benefit management. Each benefit has unique criteria for qualification, such as the applicant’s age, income, expenses, or number of household members. It can be time-consuming to confirm whether the applicant meets all of the requirements, and when they do, you also have to calculate the correct benefit amount they should receive.
For example, a constituent’s eligibility for the LIHEAP benefit depends on whether their household income falls within a qualifying threshold, and the threshold increases for each additional resident.

With Benefit Management, you can automate complex eligibility calculations so that constituents can identify benefits they may be eligible for. By entering a few key details in a prescreening form, constituents can quickly see a list of the benefits and programs for which they meet the base criteria. Benefit Management comes with a sample prescreening form that you can configure to assess eligibility for the benefits your agency administers.
Application reviewers can also use eligibility assessments to speed up their reviews. By clicking the Check Eligibility button on the application record, the reviewer can automatically simulate the benefit amount that the constituent qualifies for based on the submitted data.
Eligibility Calculations
In the last unit, you saw how Omniscripts capture prescreening and application data from constituents using Omniscript forms in the Benefits Assistance Portal. To automate eligibility calculations based on this input data, use these two components of Business Rules Engine.
- A decision matrix (or lookup table) contains the eligibility criteria for a benefit in rows of inputs and outputs.
- An expression set compares the inputs that the constituent enters in the Omniscript form to the values in the decision matrix and produces a detailed result.
Decision matrices and expression sets accept inputs from and return outputs to Omniscripts in JSON format.
Benefit Management provides out-of-the-box decision matrix and expression set templates to speed up configuration. Here’s an example decision matrix that stores the criteria for LIHEAP eligibility checks. This decision matrix organizes the eligible amounts by household size.

Notice the two currency columns for income: one for three-point limits and another for two-point limits. More on that in a second.
When the constituent selects Submit on the application form, the expression set shown here automatically determines eligibility and qualified amounts.

The constituent enters the income amount and household size in the Omniscript form. Then, the expression set assesses the form entries against the income limits in the decision matrix.
In addition to assessing household size and income, the expression set assigns weight to certain input information based on program policy. For example, the calculation step shown here assigns two points if children reside in the applying household.

If the Check If There Are Children in the Household condition is true, the maximum allowable benefit amount increases for the applicant.
As with the Omnistudio templates, you can adjust these components or create your own to reflect the eligibility parameters for the benefits your agency offers.
Automation is great for speeding up eligibility determination, but it’s also important for caseworkers to be able to share with constituents the reasoning behind decisions. Decision Explainer makes the decisions transparent. Set up Decision Explainer components, including explainability action definitions, to quickly provide insight into policy decisions and take the guesswork out of complex business-rule calculations.
To learn the steps for setting up automatic eligibility calculations and using Decision Explainer in your org, Automate Eligibility Determinations in Salesforce Help.
Benefit Review
To stay compliant and ensure the proper allocation of resources, benefit applications typically require analysis by agency personnel. With Benefit Management, intake officers, caseworkers, and case managers can systematically review applications and easily check whether constituents meet eligibility requirements for the benefits they seek.
With the Benefit Review Guided flow, reviewers can:
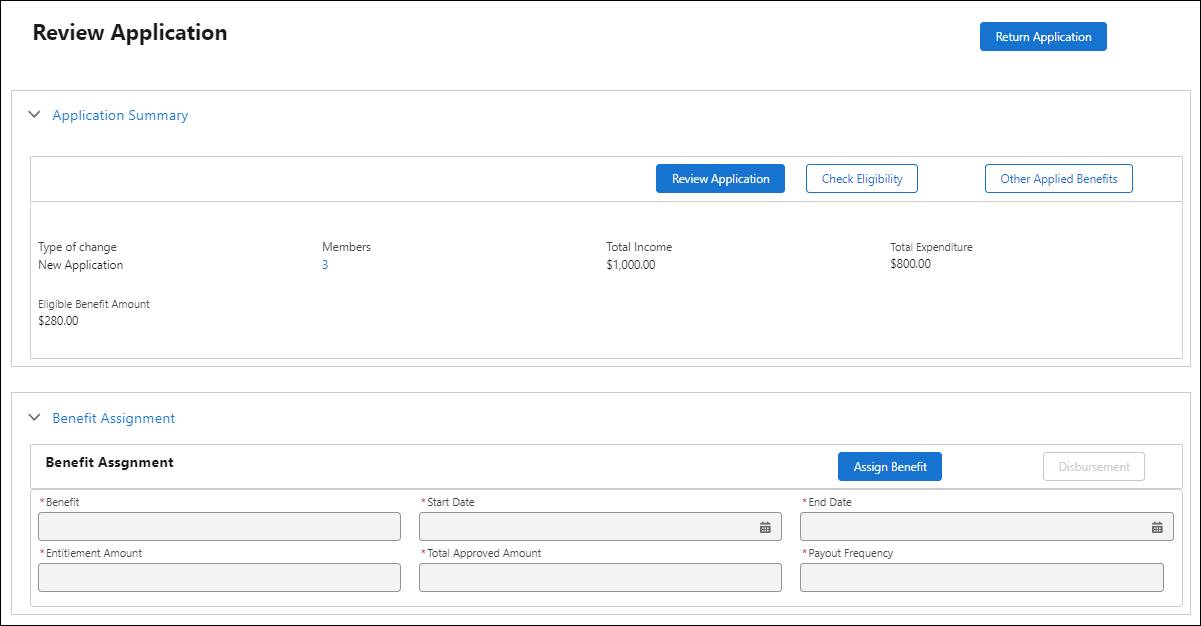
- View a summary of constituent details, including their household size, monthly income and expenses, and an estimated qualified benefit amount.
- Quickly return applications that lack important information.
- Update details based on reported changes in the constituent’s circumstances.
- Automatically perform calculations to check constituent eligibility.
- Assign and disburse benefits to eligible applicants.
Here’s a look at the Review Application Omniscript Flexcard on the application record.
To set up the benefit-review guided flow, activate Omniscripts, Data Mappers, and Integration Procedures, which add, fetch, and update application information. Then, add the guided flow Flexcard to the application record page. You can also set up queues to automatically route applications to the next reviewer based on their role. The next reviewer in the queue receives an alert when it’s their turn to review the application. To view the full set of configuration steps, see the link in the Resources section.
Change of Circumstances
Constituents must typically notify the agency when life events affect their benefit eligibility. For instance, increased income might disqualify a household, while decreased income or an additional member could increase benefits. Reporting these changes often requires a phone call with long hold times or submitting an entirely new application.
Benefit Management includes a configurable guided flow that benefit recipients can use to quickly report changes in their personal, household, or financial circumstances. In their benefits portal, constituents can view their current details, make updates to specific fields, and upload supporting documents.
On the back end, Benefit Management creates a change of circumstances application that provides the caseworker with an overview of the changes. The caseworker can then quickly assess the constituent’s eligibility based on the new information. If the caseworker approves the application, the system automatically updates the necessary objects with the new application information, generating a new application for each impacted benefit.
The change of circumstances guided flow uses an Apex class, Integration Procedures, Data Mappers, and Omniscripts. To learn how to set up the Benefit Review and Change of Circumstances guided flows, see the links in the Resources section.
You’re well on your way to streamlining your agency’s benefit management. The final setup task is to configure the benefits portal, which you explore in the next unit.
Resources
- Trailhead: Business Rules Engine
- Salesforce Help: Set Up the Eligibility Assessment Flow for Your Benefit Assistance Site
- Salesforce Help: Set Up the Benefit Application Review Flow
- Salesforce Help: Create a Queue for Application Reviewers
- Salesforce Help: Set Up the Change of Circumstances Application Flow