Discover Utilization Management for Providers
Learning Objectives
After completing this unit, you’ll be able to:
- Describe the key users of utilization management for provider organizations.
- Describe how Utilization Management for Health Cloud automates need assessment and authorization submission.
Utilization Management for Providers
With Utilization Management for Health Cloud, providers can:
- Submit and track authorization requests electronically through electronic prior authorization (ePA), eliminating the need for manual paperwork and phone calls
- Verify eligibility and benefits upfront to eliminate the primary cause of administrative denials
- Get real-time visibility into the status of submitted requests
- Gain insight into submitted prior authorization (PA) requests to help improve operations
- Drive interoperability between Electronic Health Record (EHR) and Health Cloud for creation of PA requests
The utilization management process typically begins with need assessment, in which the provider determines whether a specific medical procedure or service requires a PA request. Remember, PA is the process for determining whether a medical procedure or service is medically necessary and is covered under the patient’s insurance plan.
If a procedure requires PA, then the provider submits the request to the patient’s insurer. If a procedure doesn’t require authorization, then the provider can immediately perform the desired service with the assurance that it will be covered by the patient’s insurance.
Common medical procedures that typically require PA include many imaging tests, surgical procedures, specialty medications, rehabilitation services, and mental health services. Other procedures, such as routine office visits, preventive care, diagnostic tests, and simple surgical procedures, sometimes don’t require PA. However, these authorization requirements can be quite complex and vary based on the insurer, the insurance plan, and the specific medical procedure or service.
It is critical, then, to create a consistent, user-friendly, automated experience to easily determine whether PA is required for a given set of characteristics. And when a PA is required, there must be a similarly straightforward process for the submission of any needed authorizations. Otherwise, providers can get bogged down in an administrative back-and-forth with the payer that delays care and increases cost.
Need Assessment
To see how Health Cloud can help streamline and automate providers’ UM requirements, meet Charles Green, a member of Cumulus Health Plans, which is a large health insurance company. Charles has a chronic hip condition that has never been properly treated.

Charles’s in-network orthopedist has prescribed a series of physical therapy sessions at his clinic to treat his hip pain. The clinic uses Health Cloud to handle its authorization management processes.
Thomas Boon, the authorization coordinator at the clinic, handles all need assessment and PA requests. In his role, the coordinator:
- Checks the need for PA of medical services
- When PA is required, submits PA requests with required details and attachments to the payer
- Follows up on the status of any submitted request
- Coordinates on requirements raised by the payer to enable decision
- Facilitates peer-to-peer reviews between payer and provider
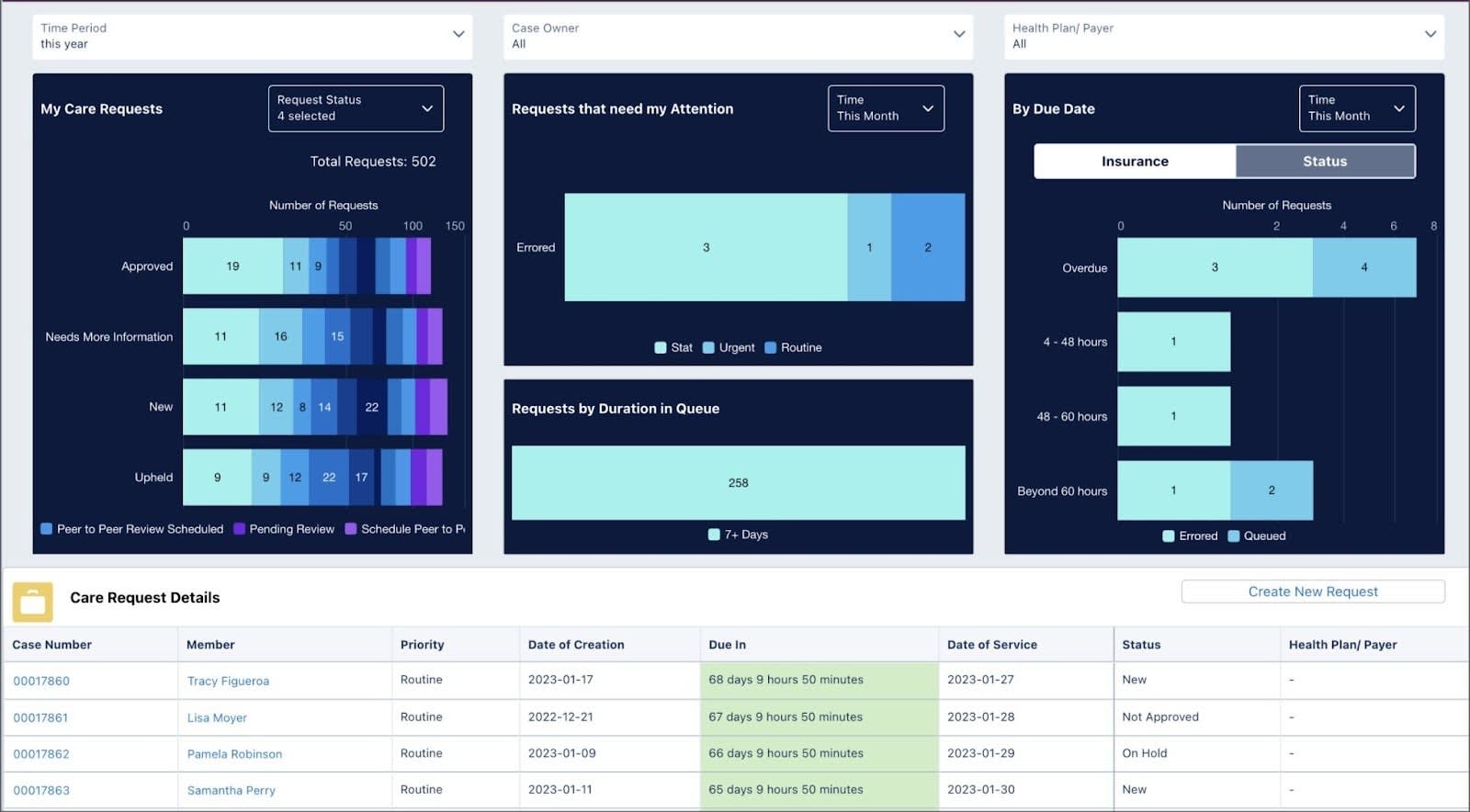
Thomas starts his day visiting a handy dashboard to view current care requests and create new requests.
Thanks to Mulesoft Direct for Health Cloud’s EHR Connector, Thomas can easily pull patient and clinical data into his Health Cloud org.
And on the payer side, Cumulus Health Plans uses Business Rules Engine (BRE) tools to determine whether PA is required for any service request. Prebuilt rule templates make it a breeze to customize rules to fit their specific requirements.

For more information about configuring business rules, check out the Business Rules Engine module.
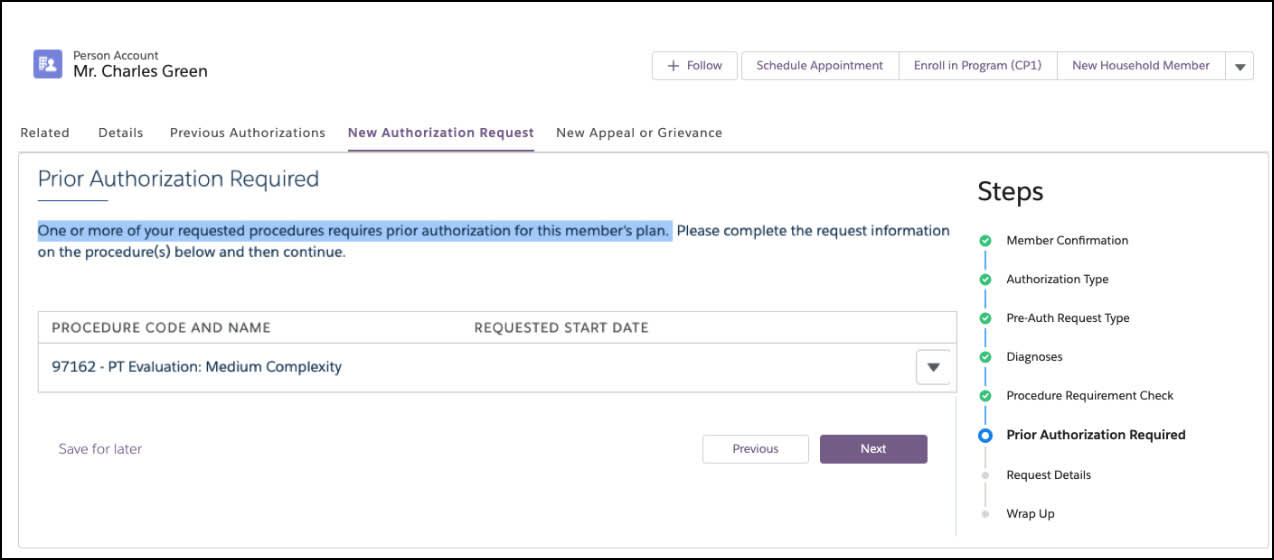
Based on the information Thomas provides, the system notifies him that Charles’s hip procedure requires PA.
Throughout the process, the authorization coordinator uses CRM Analytics to view key metrics, track all authorizations, and manage payer requirements for supporting information.
Next up, submitting the authorization request.
Authorization Submission
Healthcare providers can use out-of-the-box guided processes, combined with Mulesoft’s EHR connector, to submit an electronic prior authorization (ePA) request in Da Vinci FHIR R4 format.
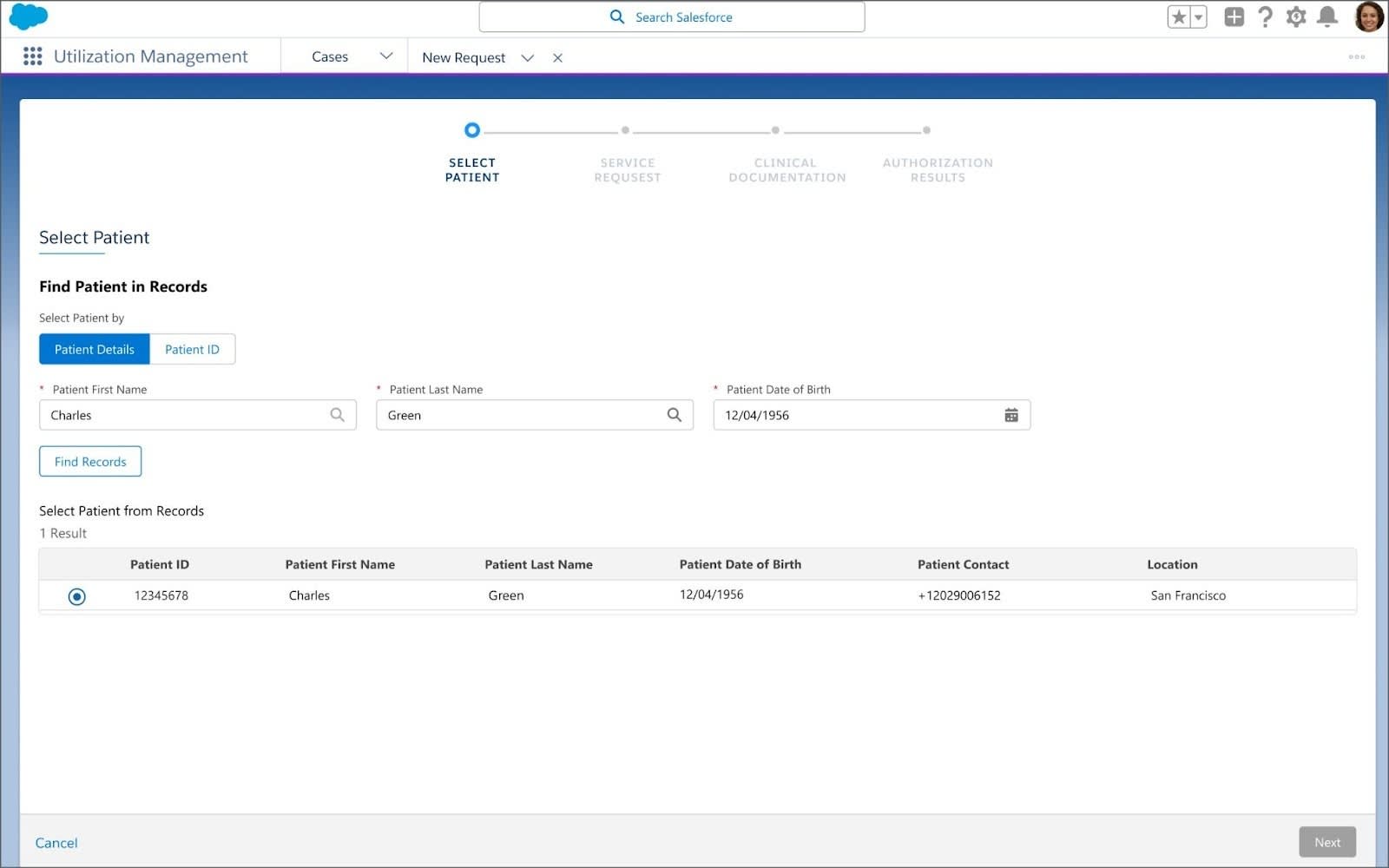
For the physical therapy request, Thomas launches the authorization workflow from his dashboard, selecting Charles as the patient.
Next, Thomas adds key details about the specific request, including provider details and service codes.
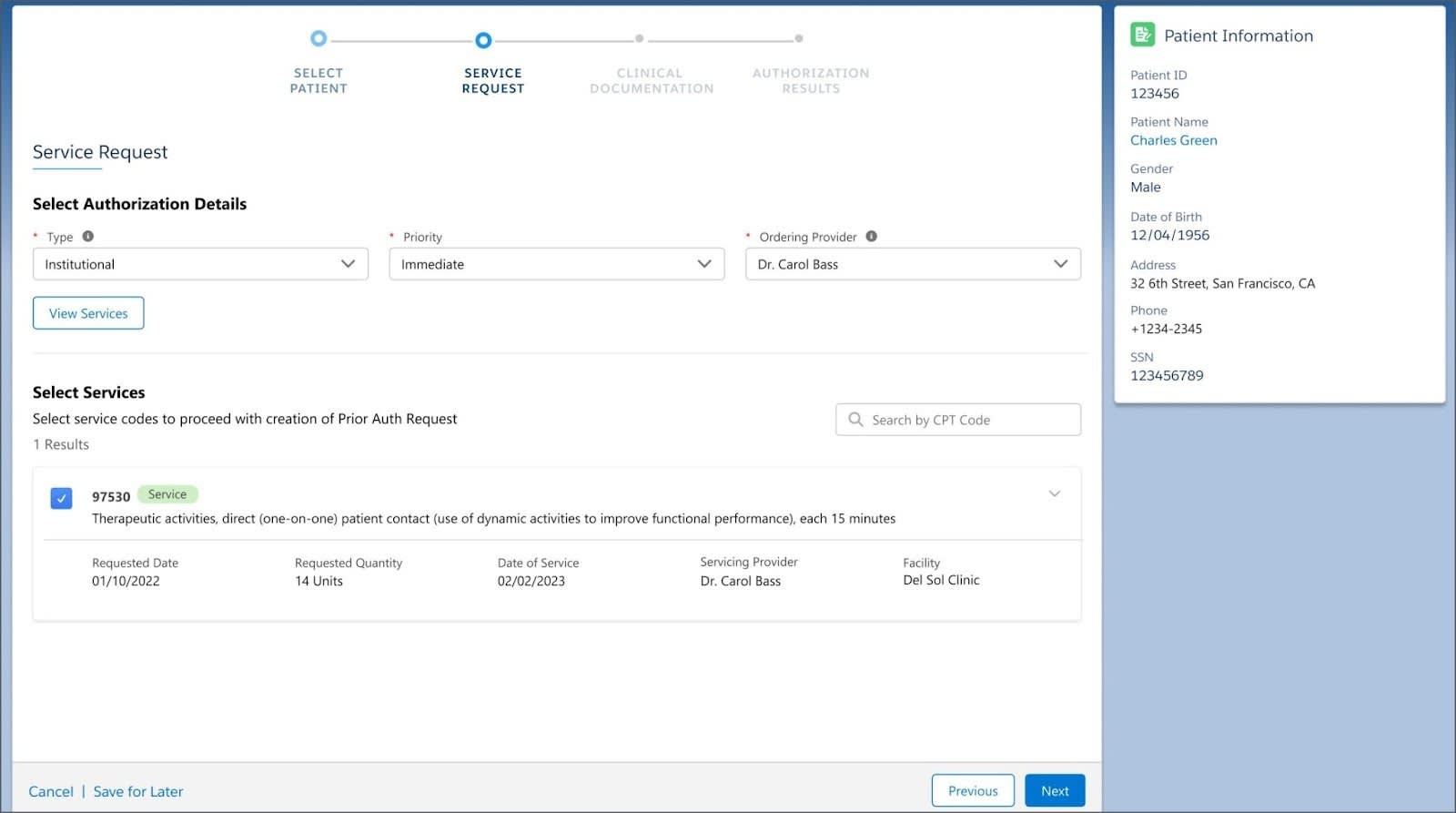
After he selects the appropriate authorization details and services, Thomas then uploads all required documentation and adds Charles’s insurance information.
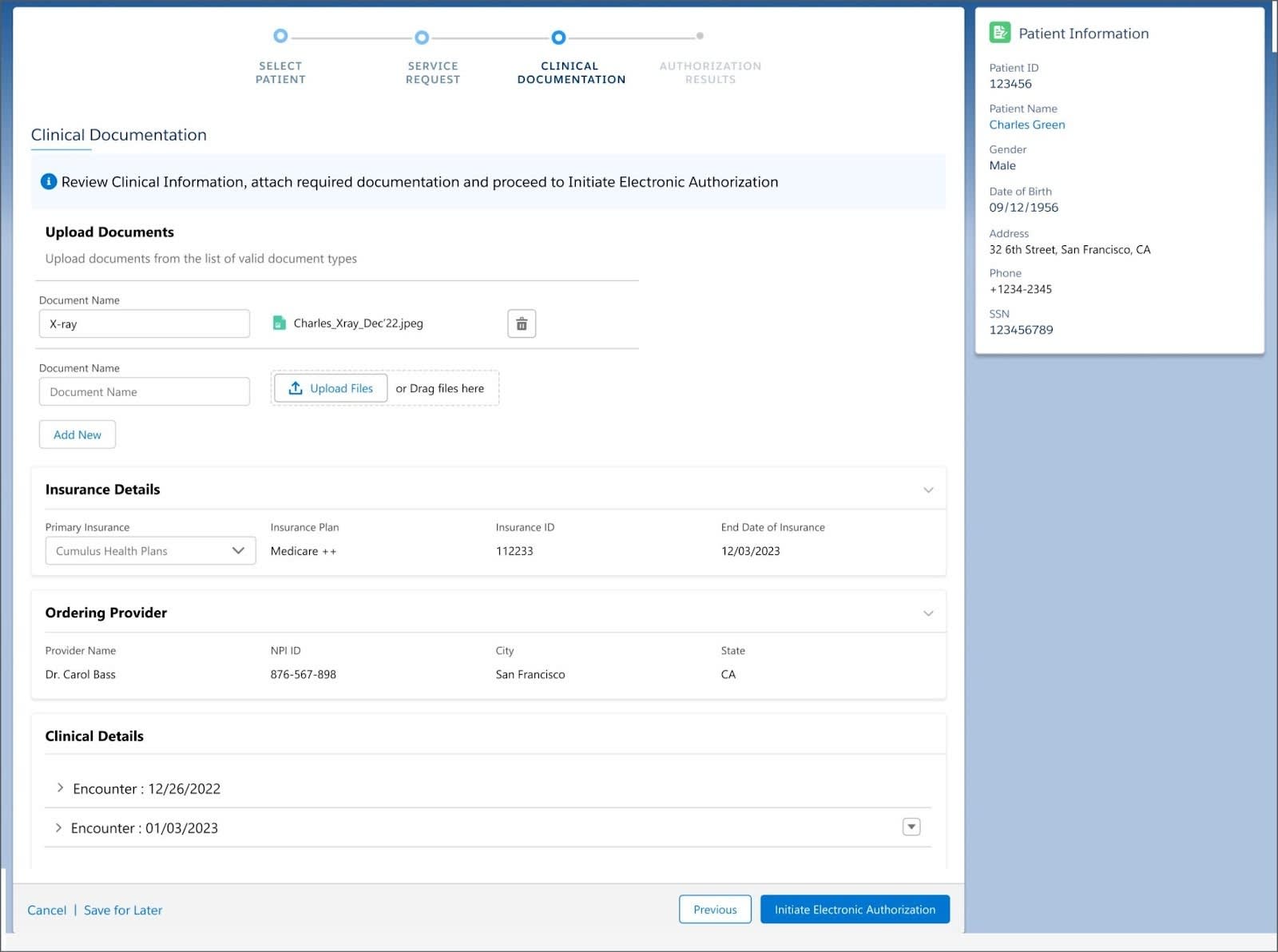
On the payer side, Cumulus Health Plans has set up auto-approval rules that can provide instant determination on the request or send the request for a full clinical review. Because the request is submitted in FHIR R4 format, Cumulus can then easily intake the request from the FHIR endpoint.
Based on preset criteria, authorization for Charles’s visits is instantly approved!
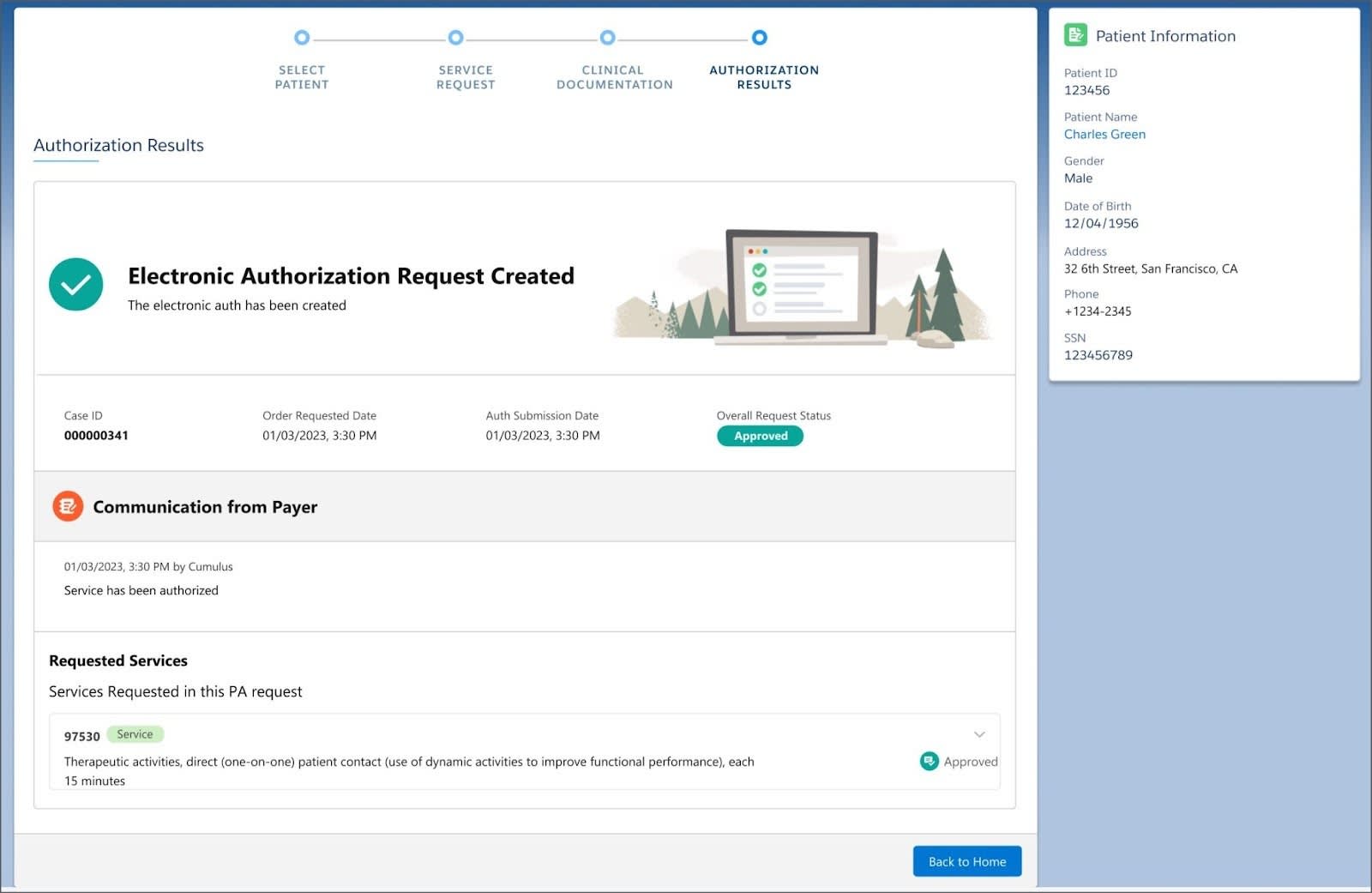
From the authorization results screen, Thomas can view any communication from the payer and confirm details about the requested services. Providers can also take advantage of AI-based Recommended Services Bundling to anticipate child authorization requests for additional services based on historical patterns. This further reduces administrative delays for care delivery.
After Thomas receives the authorization approval, he visits Charles's patient record, where he can view all his authorization requests and instantly schedule the approved physical therapy sessions.

You saw how Health Cloud greatly streamlines and simplifies the authorization submission process for providers. But how does it assist payers?
In the next unit, you learn how payers use Health Cloud to handle complex, offline authorization requests and smoothly navigate the intake, review, and decision stages.
Resources
- Salesforce Help: Create and Submit Authorization Requests to Payers
- Salesforce Help: Built-In MuleSoft Integration to Manage Authorization Requests
- Salesforce Help: Recommended Services Bundling for Providers