Investigate the Health Insurance and Claims Data Model
Learning Objectives
After completing this unit, you’ll be able to:
- Explain the purpose of the Health Insurance and Claims data model.
- Describe the objects related to purchaser plans.
- Describe the objects related to member plans.
- Describe the objects related to claims.
The Health Insurance and Claims Data Model
The Health Insurance and Claims data model provides objects for managing the ways healthcare is paid for. These objects represent information about members and their employers, insurance coverage, and dependents. This data model includes objects for claims submitted to a member’s health insurance company by an entity or person who provides a service, medication, or device to the member.
Charles has a health plan through his employer, Get Cloudy Consulting, which is a global company that has purchased a health insurance plan from Bloomington Health Plans, a payer organization.
Bloomington Health Plans offers health insurance tailored to Get Cloudy Consulting for its US-based employees. Charles opted to enroll in Bloomington Health Plan’s preferred provider plan (PPO). As part of his policy, Charles is entitled to Rehabilitative Services, which includes up to 30 physical therapy visits per year.
Let’s first examine the objects that represent the purchasing organization (Charles’s employer) and the plan they purchase from the payer organization.
Purchaser Plans
Get Cloudy Consulting’s US Employees purchaser group purchases a health plan from Bloomington Health Plans. The plan includes rehab services as a benefit.
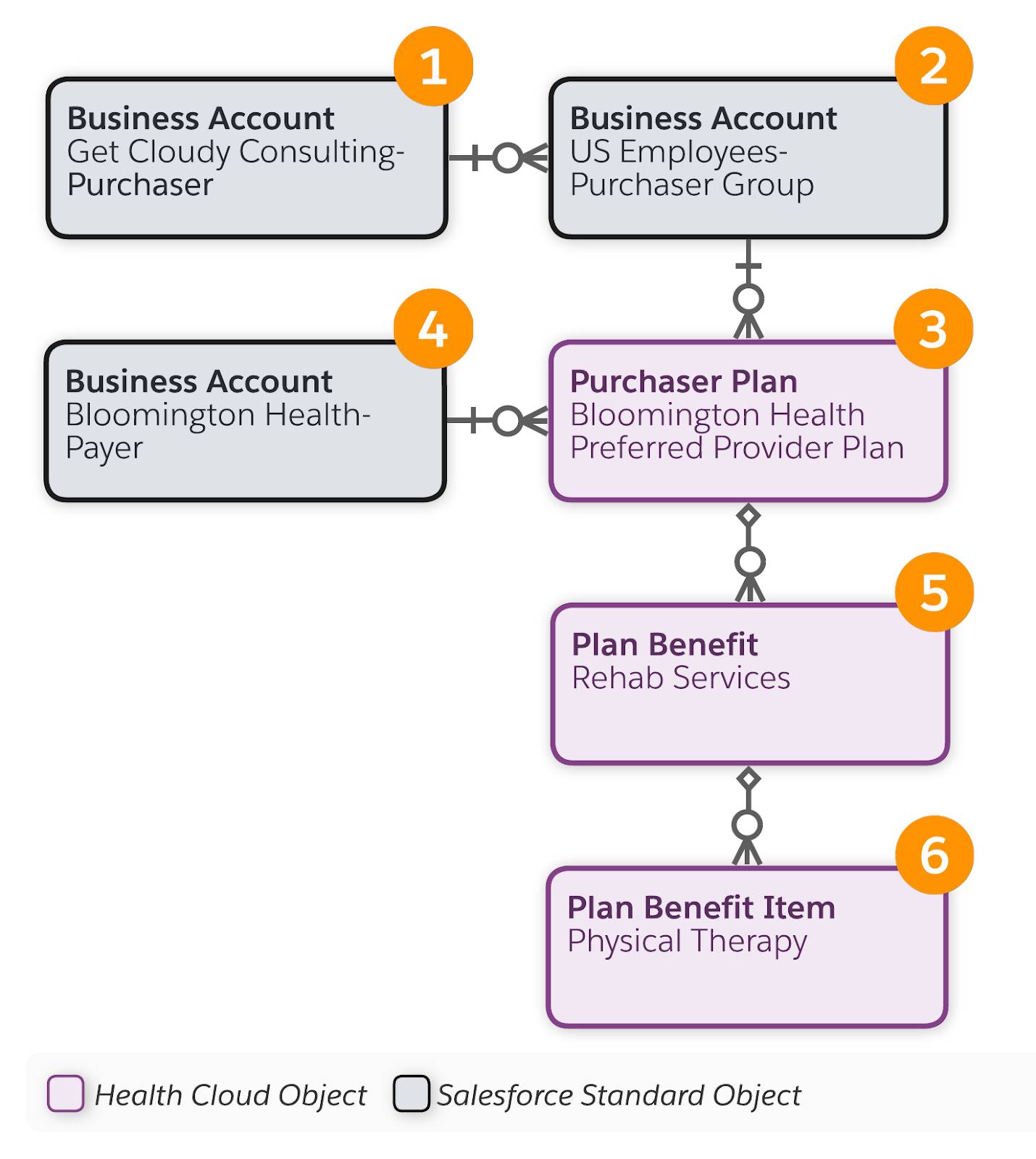
Here’s a summary of the objects and records.
Scenario Details |
Object and Record Details |
|---|---|
Get Cloudy Consulting is a global company that has purchased a health insurance plan for its US-based employees. |
The Account object with a Business record type (1) represents the organization (purchaser) that purchases the health plan. The Account object also represents purchaser groups that are subsets of the purchaser (2). For example, an organization may have employee groups in different countries or different regions of a country. Each purchaser group can have separate options for insurance plans. The account record for the purchaser group references the account record for the parent organization. |
Bloomington Health Plans offers health insurance tailored to Get Cloudy Consulting for its US-based employees, such as a Preferred Provider Plan (PPO). |
Purchaser Plan (3) represents the plan that a purchaser makes available to its members and members’ dependents. A purchaser plan record references a purchaser or purchaser group record and the payer record. |
Bloomington Health Plans is a payer organization that provides health insurance plans. |
The Account object with a Business record type (4) represents the payer organization that helps cover the cost of member care. |
Bloomington Health Plans offers Rehab Services as a benefit. |
Plan Benefit (5) represents the standard benefits available under a plan that the purchaser offers to their members. A plan benefit record references a purchaser plan record. |
Bloomington Health Plans offers physical therapy visits as part of its Rehab Services benefit. |
Plan Benefit Item (6) represents the details of a benefit. A plan benefit item record references a plan benefit record. |
Now let’s examine the objects that represent the member and the member plan they subscribe to.
Member Plans
As a US-based employee of Get Cloudy Consulting, Charles Green subscribes to a member plan that includes rehab services as a benefit.
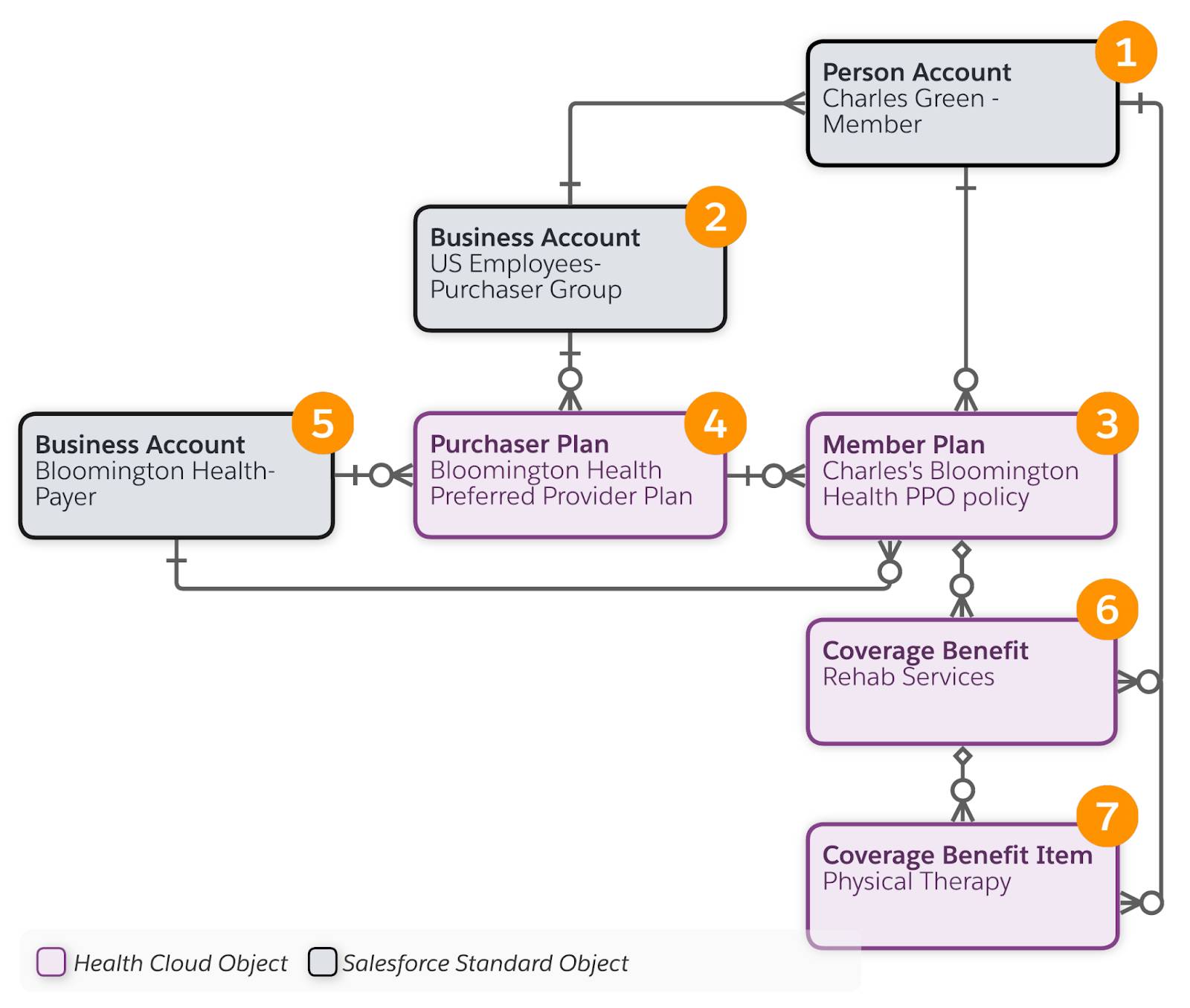
Here’s a summary of the objects and records.
Scenario Details |
Object and Record Details |
|---|---|
Charles Green is a member who is covered under an insurance plan. |
The Account object with a Person record type (1) represents a member. A member has a relationship with the purchasing organization (2). For example, the member is an employee and the organization is their employer. |
Charles enrolled in Bloomington Health Plan’s preferred provider plan (PPO). |
Member Plan (3) represents details about the insurance coverage for a member. A member plan record includes data such as the plan effective dates, the group number or policy number of the primary member, and the plan’s verification status. A member plan record references a purchase plan record (4) and the payer organization (5). |
As part of his policy, Charles is entitled to Rehabilitative Services. |
Coverage Benefit (6) represents the coverage benefits that a member plan provides to a covered member. A coverage benefit record includes data such as the benefit period start and end dates, the coverage type (Dental, Medical, Vision), and deductible limits. Each coverage benefit has a benefit item. |
This benefit includes up to 30 physical therapy visits per year. |
Coverage Benefit Item (7) represents the specific services that a member plan covers. A coverage benefit item record includes data such as the type of service it provides, and whether or not the service must be preauthorized before use. |
Now that we’ve looked at the health insurance objects, let’s move to the objects that represent the claims process.
Claims
Claims data resides outside Salesforce in a 3rd-party system. The Health Cloud claims functionality is delivered as an unmanaged package that contains a set of external Claim objects. External objects are objects that map to data that’s stored outside your Salesforce org. External objects enable your users to search and interact with the external data.
Before you install the Claims package, make sure your organization has a Salesforce Connect license. You need Salesforce Connect to set up the connection to your source system so that Health Cloud can pull your organization's claims data into the external objects. You need middleware to get this data from the 3rd-party claims systems.
In Setup, go to External Objects to view the claims objects and open them in Object Manager. You won’t see the objects if you search for them in Object Manager itself.
Sara Johnson is the physical therapist who provides therapeutic exercises to help Charles address his back pain. Sara files a claim for providing this service.
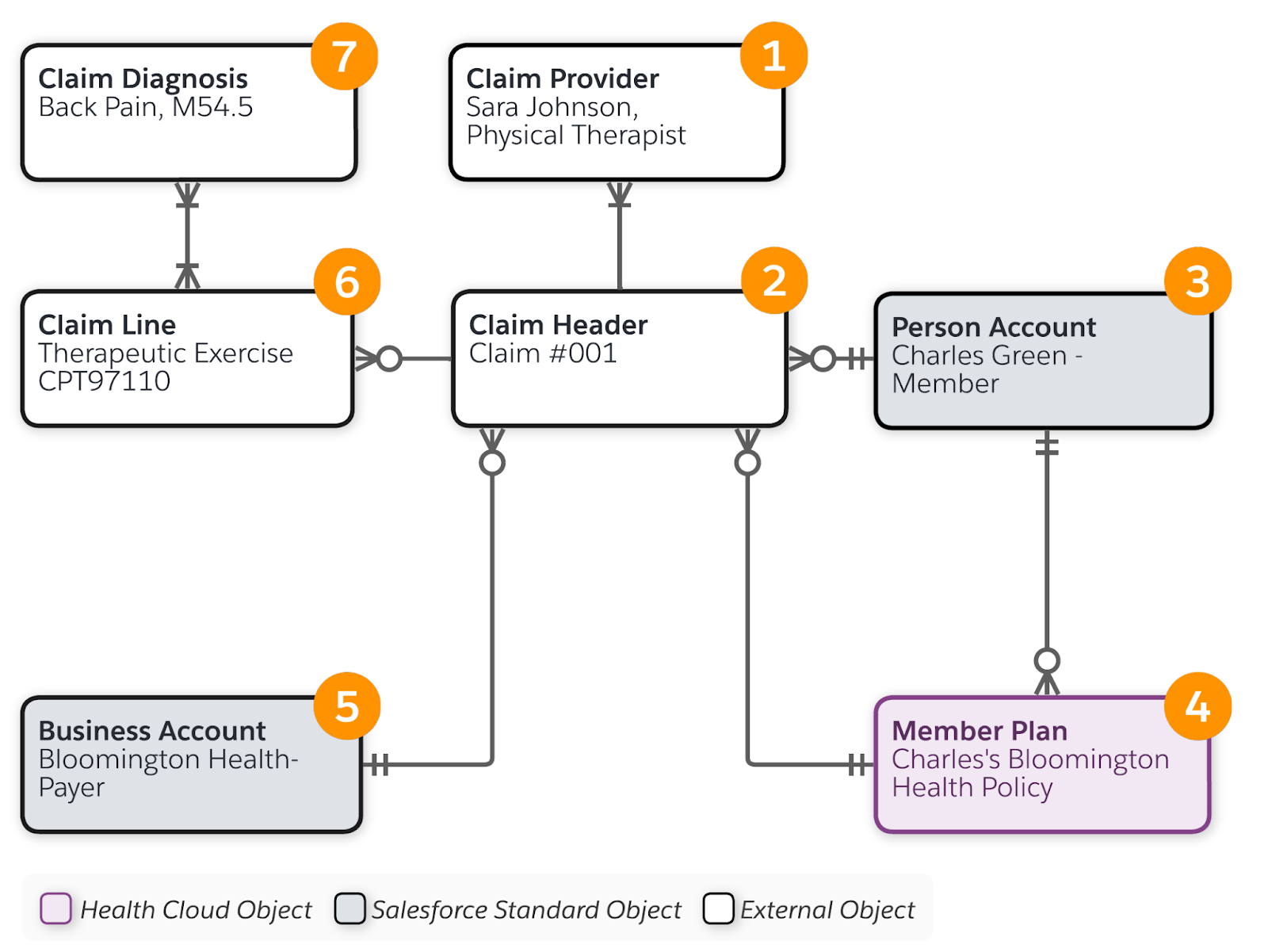
Here’s a summary of the objects and records.
Scenario Details |
Object and Record Details |
|---|---|
Sara Johnson is the physical therapist who provides therapeutic exercises to Charles. |
Claim Provider (1) represents information about a provider of a service, equipment or medication. |
Sara files a claim for providing this service. |
Claim Header (2) contains summary information about the claim, such as the payment amount, specified medications, and billing data. A claim record references the provider who’s submitting the claim (1), and the member (3), member plan (4), and payer organization (5). Claim Line represents a line item in a claim record (6). In this example, the claim is for the Therapeutic Exercises that Sara provided. A claim line record references a claim diagnosis record. |
The therapeutic exercises are to help Charles with his back pain. |
Claim Diagnosis (7) represents the clinical diagnosis for which the service, equipment, or medication was provided. In this example, Back Pain is the diagnosis. |
For more details about the objects we introduced in this unit, see the Salesforce Health Cloud Developer Guide.
Next, let’s learn about the objects that come into play when Charles enrolls in a care program.
Resources