Understand the Utilization Management Data Model
Learning Objectives
After completing this unit, you’ll be able to:
- Explain the purpose of the Health Cloud Utilization Management data model.
- Describe the objects for care requests.
- List additional Health Cloud data models for healthcare.
The Utilization Management Data Model
Utilization Management (UM) is the use of managed care techniques such as prior authorization to allow payers to manage the cost of health care benefits by assessing a benefit’s appropriateness before it’s provided, using evidence-based criteria or guidelines. UM ensures that patients receive the right care, at the right time, for the appropriate duration, in the right setting.
In Health Cloud’s Utilization Management, OmniStudio components combine to provide a guided user interaction for users who manage authorization request submissions and reviews. OmniScripts are available to create and submit an authorization request, conduct admin, nurse, and medical director reviews of the authorization request, and conduct peer-to-peer reviews with the requesting provider.
Business Rules Engine components streamline approval processes, simplify complex lookups, and automate business decisions in the authorization request workflows.
The UM data model aligns with FHIR R4 for interoperability and integration with external systems. UM includes APIs and integration applications deployed on MuleSoft for uninterrupted request processing with external Electronic Health Record (EHR) and payer systems. These APIs align with the FHIR Da Vinci Health Record Exchange (HRex) implementation guide.
The Utilization Management data model provides objects for evaluating care requests such as preauthorization requests and prescription or medical service requests. This unit uses a preauthorization request as an example.
When Charles Green visits physical therapist Sara Johnson for the first time, Sara determines she needs 10 physical therapy sessions to treat his lower back pain.
Sara submits a preauthorization request for the sessions to Bloomington Health Plans, Charles’s health insurance plan. She provides the necessary details for Bloomington Health Plans to evaluate the request (case).

Melinda Smith is a utilization management nurse at Bloomington Health Plans. When Melinda evaluates the request, and based on medical necessity guidelines, she ascertains that the request should be approved. She refers the preauthorization request to Dr. Barbara Brown (Medical Director) to confirm approval. Dr. Brown evaluates the request, and based on Charles’s clinical history, she approves the request.
Let’s map this scenario to the objects in the Utilization Management data model.
Care Requests
Sara submits a preauthorization request for Charles’s physical therapy sessions to Bloomington Health Plans. The Care Request, Care Request Extension, and Case entities capture the authorization request details.
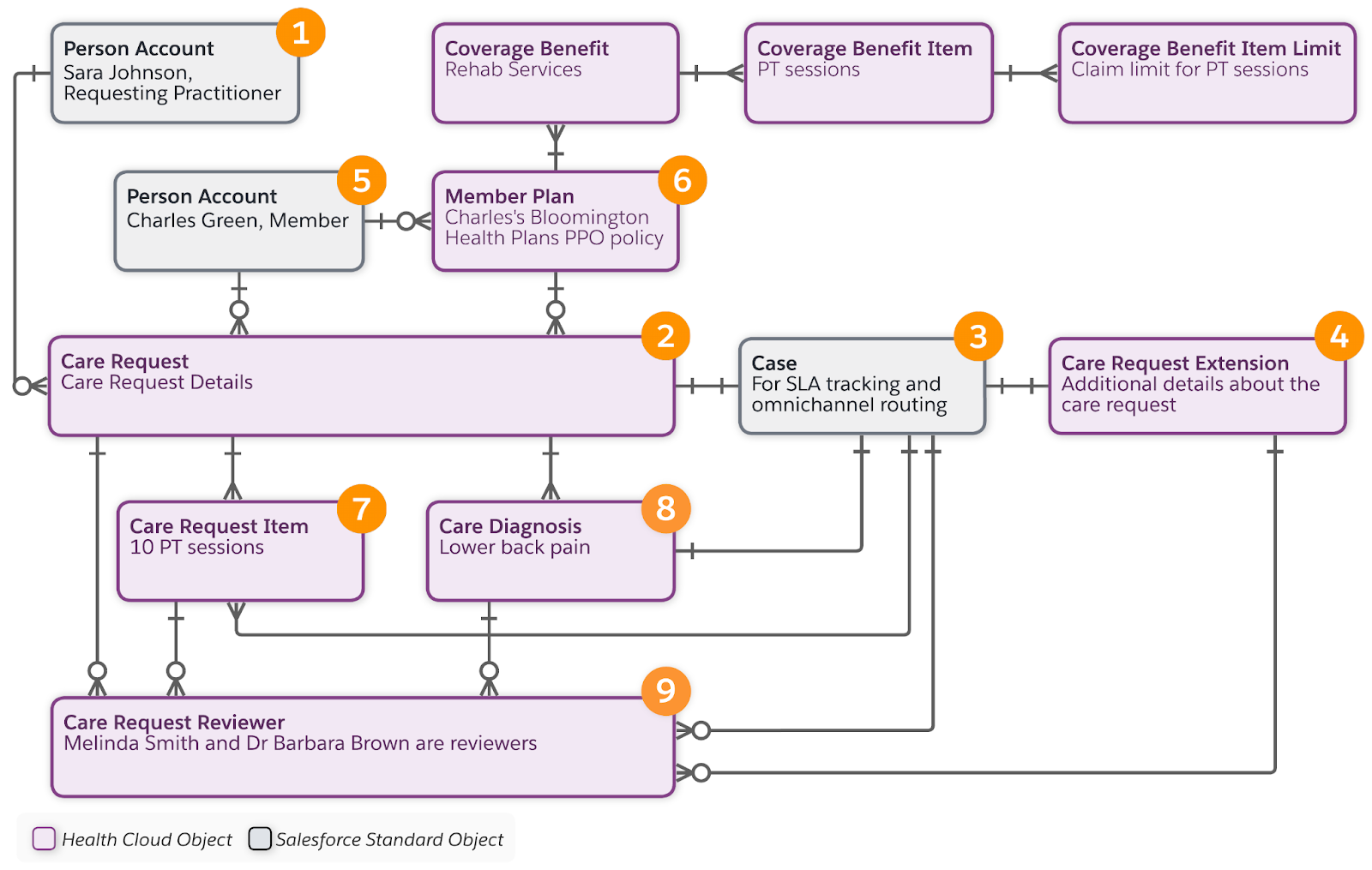
Here’s a summary of the objects and records.
Scenario Details |
Object and Record Details |
|---|---|
Sara Johnson is the practitioner who requests a preauthorization |
The Account object with a Person record type (1) represents the requesting practitioner and servicing practitioner. The requesting and servicing practitioners can be different people but in this example, Sara is doing it all. |
Sara Johnson submits a preauthorization request. |
Care Request (2) represents the general details of a care-related request. Care requests include preauthorizations for drugs and services, admission notifications, and concurrent reviews of admissions. A single request can contain multiple diagnoses and services. |
Sara’s preauthorization request generates a case record. |
Case (3) represents the case record for the preauthorization. This object allows for setting up SLA tracking based on milestones and entitlements, and omnichannel routing for workflow management. |
Sara’s preauthorization request includes additional details related to the member’s health plan. |
Care Request Extension (4) represents extra details for a care request such as subscriber details for the member's health plan. |
Charles is the member who needs care. |
The Account object with a Person record type (5) represents Charles Green as a member. |
Charles subscribes to the Bloomington Health Plans PPO member plan, which includes benefits for rehab services. |
Member Plan (6) represents the member plan. This object relates to the Coverage Benefit, Coverage Benefit Item, and Coverage Benefit Item Limit objects, which store the benefit details related to Charles’s member plan. |
Sara’s request includes 10 physical therapy sessions in the request details. |
Care Request Item (7) represents the details of a care service request. |
Sara refers to lower back pain as the diagnosis of Charles’ health condition. |
Care Diagnosis (8) represents the details of a diagnosis including code type, name, and description. |
Melinda Smith and Dr. Barbara Brown review the care request. |
Care Request Reviewer (9) represents the details of a care request reviewer including name, reviewer type, status of the care request at the end of the review, the reviewer’s notes, and date of review. |
For more details about the objects we introduced in this unit, and for a complete view of the Utilization Management data model, see the Salesforce Health Cloud Developer Guide.
Now that you’ve completed a virtual tour of Charles’ healthcare journey, you know the purpose of several of the healthcare data models available in Health Cloud. Well done. However, there’s more to learn!
More Healthcare Data Models
Health Cloud has additional healthcare data models that you can learn about in the Salesforce Health Cloud Developer Guide.
For each new Salesforce release, it’s prudent to pay attention to data model enhancements and updates, which occur when Health Cloud aligns with new industry standards or has new or enhanced capabilities.
Here’s a summary of the data models we didn’t cover in this module.
Data Model |
Description |
|---|---|
Benefits Verification |
Supports healthcare organizations in determining benefits coverage for services and products provided. |
Integrated Care Management |
Provides objects to store clinical data related to a patient or member’s care plans. This data model is USCDI and FHIR R4-aligned, which helps with your system’s interoperability. |
Intelligent Appointment Management |
Provides objects to help you work with multiple scheduling source systems operating on different electronic health record platforms. |
Intelligent Document Automation |
Provides objects to simplify the document management process, reduce manual data entry, and manage patient and member forms all in one place, from intake through processing. |
Remote Monitoring and Device Registration |
Provides objects for managing data collected from devices issued to patients or program members, such as smart watches and heart monitors. |
Unified Health Scoring |
The Score data model stores and processes information used for the Score List for Unified Health Scoring and Score Details for Unified Health Scoring components. The Actions data model supports displaying contextual prompts for users to act on in the Dynamic Actions for Unified Health Scoring component. |
Resources