Verify Care Benefits
Learning Objectives
After completing this unit, you’ll be able to:
- Explain the role and importance of care benefits verification.
- Describe the objects used to manage care benefits verification.
- Discuss the tools available for verifying coverage and generating benefits summaries.
Speed Up Access to Medication
Enrolling in a patient support program is just the first step—after that, patients need reliable access to their prescribed treatment. This requires verifying insurance benefits accurately, and ongoing. Without a smooth, proactive process, patients might encounter unexpected costs, prior-authorization delays, or even denials at the pharmacy counter.
Benefits verification can be a constant challenge for organizations. Payer rules, coverage criteria, and formulary requirements change all the time, making it difficult to keep coverage details up-to-date. On top of that, patient insurance plans shift due to employer transitions, annual re-enrollments, and coverage adjustments. If a change goes unnoticed, a patient who was verified just months ago can suddenly lose access to their treatment.
It’s a huge challenge because most patients face insurance changes each year, which creates an administrative burden for patient services teams. Stuck with manual processes, teams struggle to keep up, resulting in delays, errors, and frustration for both patients and healthcare providers.
PSP for Life Sciences Cloud tackles these issues head-on by automating verification and reverification to keep medication access uninterrupted.
-
Verification workflows streamline insurance checks, reducing reliance on manual processes.
-
Electronic payer integration connects directly with clearinghouses to retrieve accurate benefits data.
-
Reverification alerts and workflows detect coverage changes and proactively update patient records.
-
AI-driven communication automates outreach for missing details and updates coverages with minimal effort.
With these tools in place, life sciences teams can reduce administrative delays, maintain accurate coverage data, and help patients avoid surprise costs—all while easing the workload for patient services teams.
In this unit, you check back in with Cumulus Pharma to discover how they use Life Sciences Cloud to manage pharmacy benefits verification.
Model Benefits Verification
Care benefits verification relies on a structured data model that organizes insurance details, coverage benefits, and medication information. With this foundation, each verification request reliably links the correct patient, insurance plan, provider, and prescription—supporting fast and accurate processing.
Benefits Framework
Before verification begins, organizations define the structure of a patient’s health plan—including benefit categories, medication eligibility, and cost-sharing details.
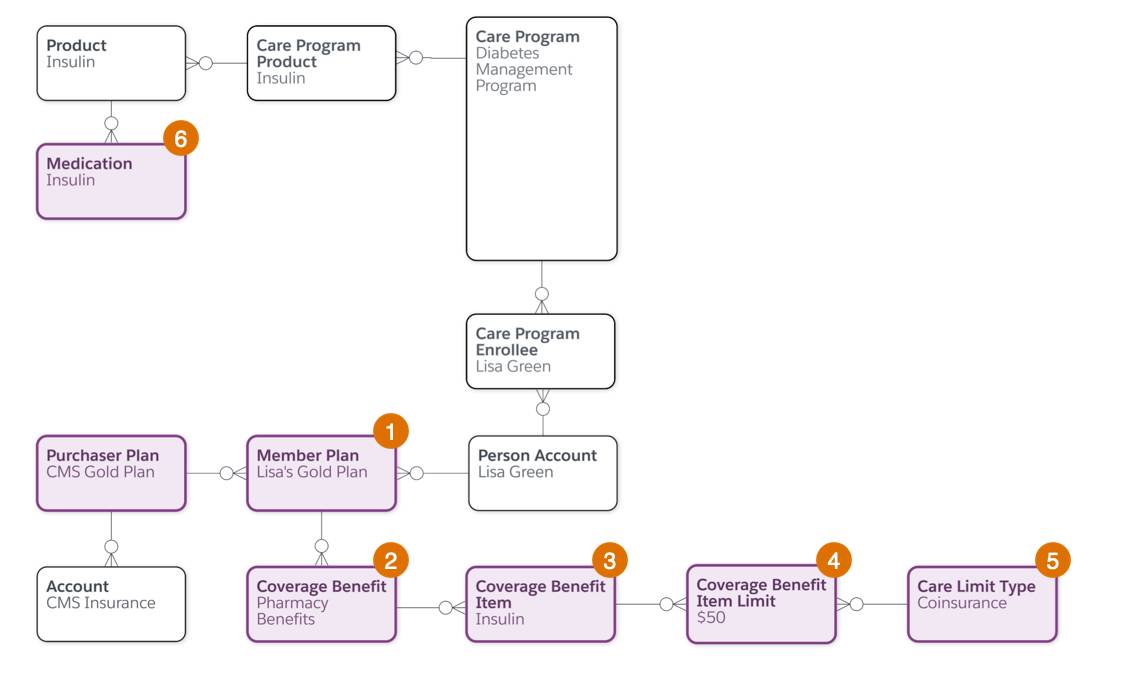
This table describes the objects and their relationships.
Object |
Description |
For example… |
|---|---|---|
Member Plan (1) |
Represents a member’s health insurance plan and links to payer information. |
Lisa’s Gold Plan links to her account. |
Coverage Benefit (2) |
Represents benefits provided under a member’s plan. |
Her Gold Plan includes prescription drug benefits. |
Coverage Benefit Item (3) |
Tracks specific covered services or medications. |
Insulin is listed as a covered item under Lisa’s plan. |
Coverage Benefit Item Limit (4) |
Specifies coverage details like copays, limits, and eligibility. |
A $50 coinsurance applies to her insulin. |
Care Limit Type (5) |
Represents the types of limits such as coinsurance and deductibles. |
The copay for Lisa’s insulin falls under the coinsurance limit type. |
Medication (6) |
Tracks detailed medication information, including quantity and dosage. |
The insulin record states her prescribed dosage and quantity. |
This structure makes coverage information easy to find and interpret during verification.
Benefits Request Records
When a patient service representative (PSR) initiates a benefits verification request, additional objects link patient insurance details with prescriber and pharmacy information. This helps ensure all approvals are handled efficiently.
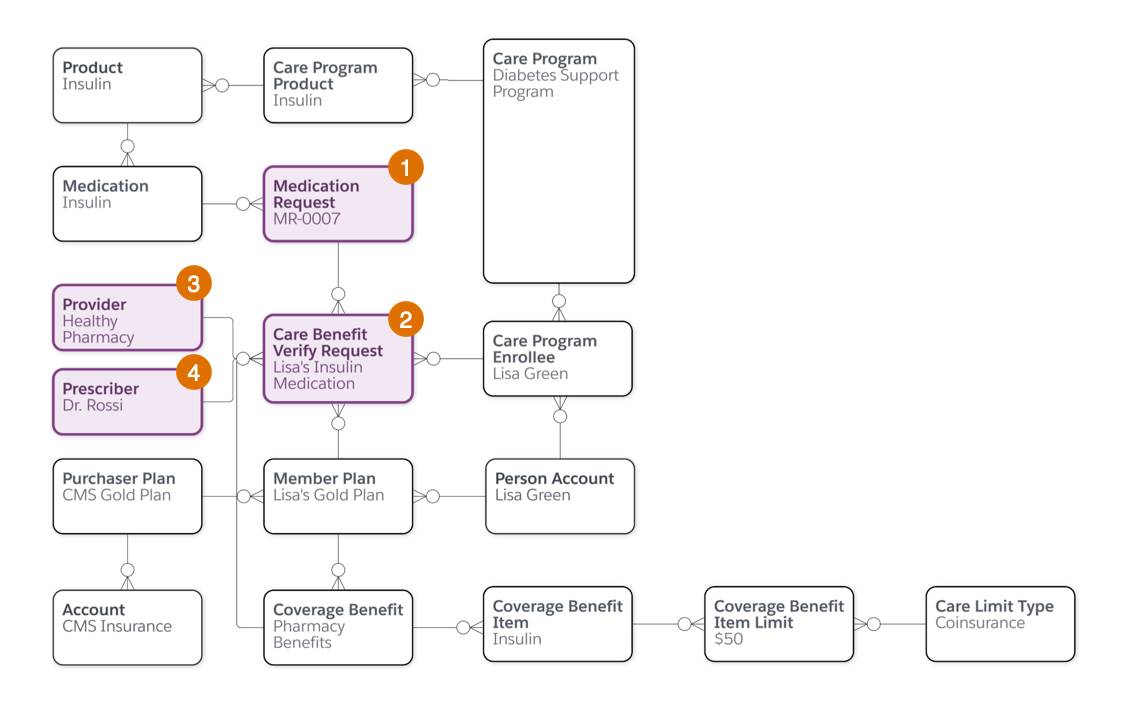
Here’s a description of these additional objects.
Object |
Description |
For example the PSR at Cumulus… |
|---|---|---|
Medication Request (1) |
Represents a request for a specific medication supply. |
Submits a request for Lisa’s insulin, including dosage instructions. |
Care Benefit Verify Request (2) |
Tracks the verification process, linking medication, plans, and payer details. |
Matches Lisa’s insulin against her Gold Plan and submits for verification. |
Prescriber (3) |
Contains information about the prescribing physician. |
Records Lisa’s doctor as the prescriber for the insulin request. |
Provider (4) |
Holds details about the pharmacy providing the medication. |
Links Lisa’s preferred pharmacy to the verification request. |
This model helps you process verification faster, stay compliant, and reduce delays.
Use Care Benefits Verification
With the data model in place, PSP shifts verification from a fragmented manual effort into a connected, automated experience. Every request is accurately assembled and efficiently processed to speed up access to treatment.
Time to follow Lief Hansen, a PSR at Cumulus Pharma, as he helps verify Lisa’s benefits.
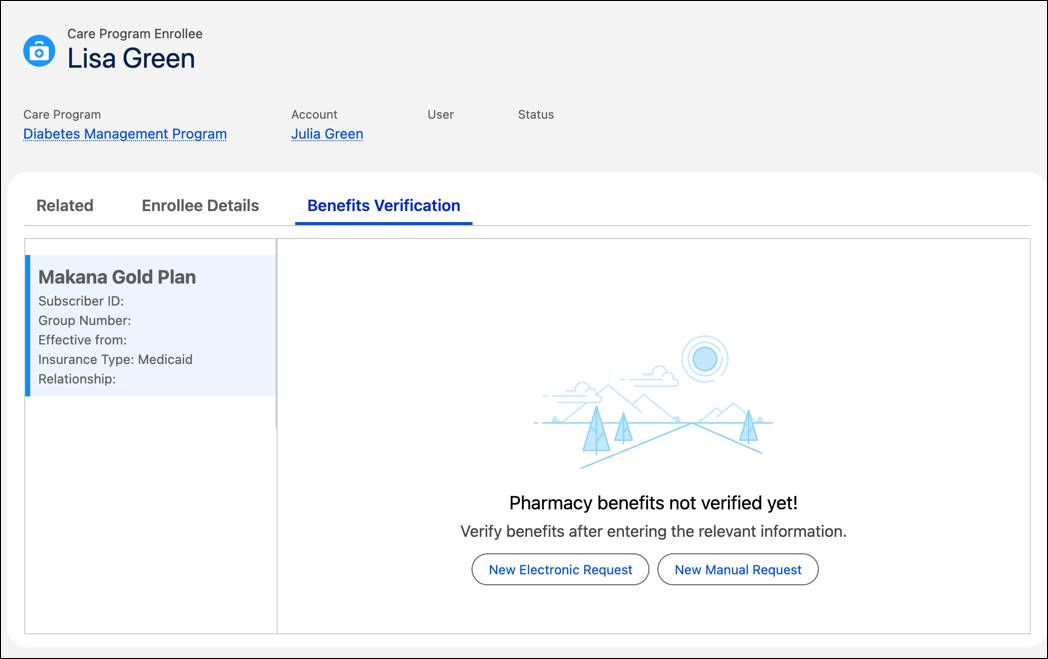
Add Member Plans
Before verification begins, Lisa’s insurance details must be recorded. Lief navigates to the Benefits Verification tab on Lisa’s record and selects Add Member Plan.
A guided flow prompts him to enter plan details like the name and member ID. Once added, the plan is tied to Lisa’s care program record, keeping all payer information in one place and ready for verification.
Verify Coverage
Lief starts the verification from Lisa’s record using one of two methods:
-
Manual Request, entering payer responses manually.
-
Electronic Request, submitting an automated request to the payer and retrieving real-time benefits data.
No matter which method is used, the guided flow automatically fills in Lisa’s drug and prescriber information—saving time and avoiding errors.
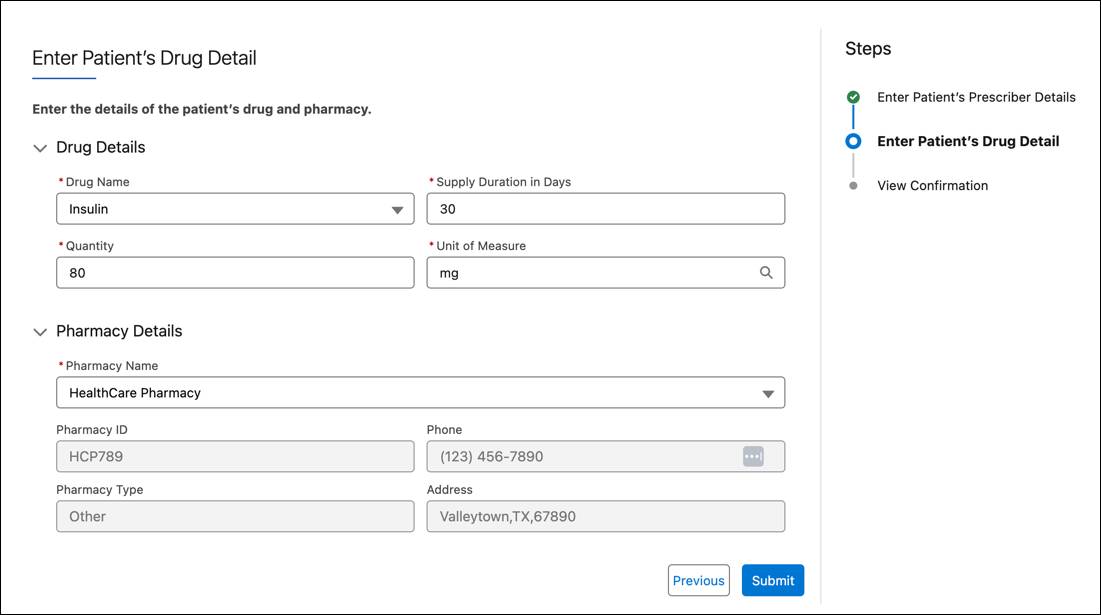
This process prevents duplication and confirms that all essential fields are completed before submission.
Organizations can tailor this verification flow by adding steps or custom fields based on payer requirements.
To learn more, check out Pharmacy Benefits Verification Request in Salesforce Help.
Manage Benefit Verification
Before submitting the request, Lief carefully reviews Lisa’s verification details, confirming that her prescription and insurance plan data align correctly.
Throughout the process, he can track payer responses directly from the Benefits Verification tab, where real-time updates ensure that benefits data remains accurate. This is done in one of two ways.
- For electronic verification, PSP automatically retrieves and displays benefits information.
- For manual verification, PSRs enter payer responses as they are received.
Lief reviews Lisa’s Benefits Summary, which outlines her medication coverage, copay, and prior authorization requirements.
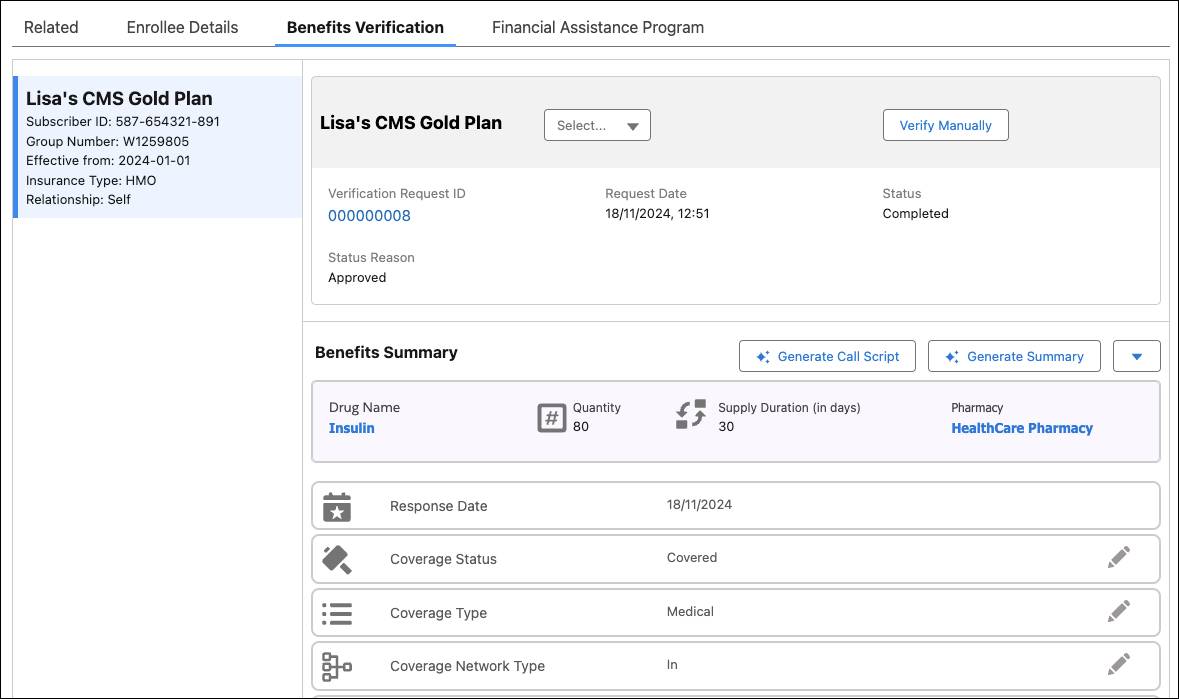
This summary provides an at-a-glance view of Lisa’s coverage, allowing her to anticipate any out-of-pocket costs or prior authorization requirements before filling her prescription.
If any details are missing or unclear, Lief uses Agentforce to generate a call script that guides a follow-up conversation with the payer.
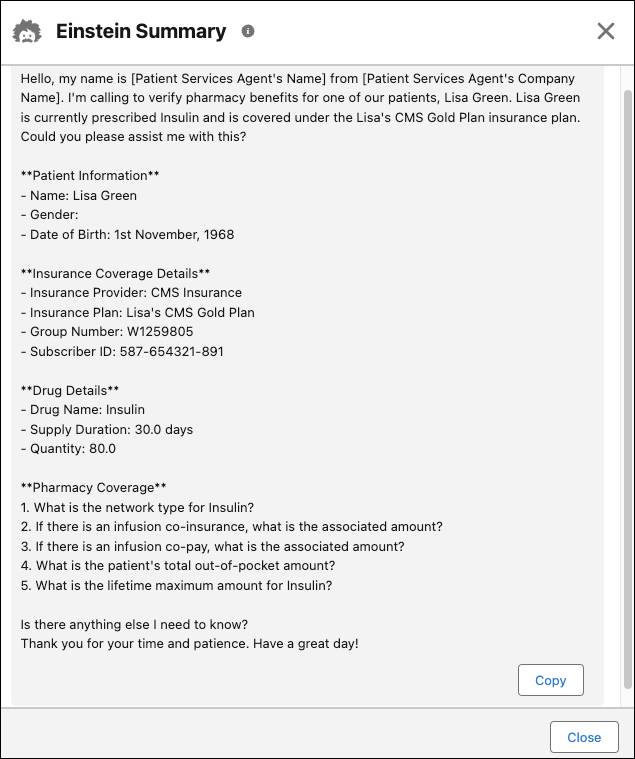
The script guides Lief through key questions, ensuring he quickly captures all the right details from the payer. After adding any missing information, he updates Lisa’s record and finalizes the benefits summary.
After verification is complete, he generates a Benefits Summary using Agentforce. The summary lists coverage confirmation, out-of-pocket costs, and prior authorization requirements.
Lisa receives the summary, giving her full transparency into her coverage before visiting the pharmacy.
For more information, see Generate Pharmacy Benefits Summary and Generate Call Script in Salesforce Help.
Manage Reverification
Medication access doesn’t stop at initial verification—insurance details frequently change, requiring timely reverification to ensure patients can continue their treatments without disruption.
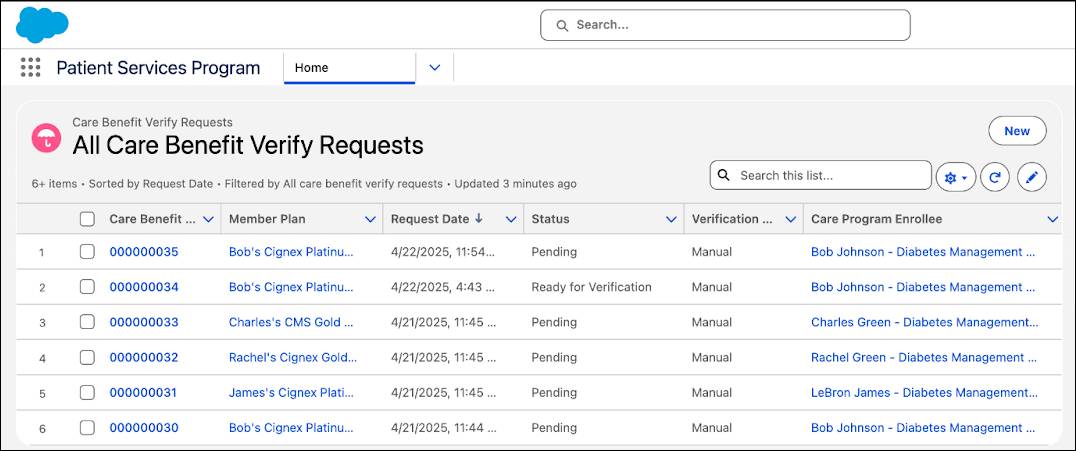
To stay ahead, Cumulus Pharma uses PSP’s automated reverification features. A program lead initiates the process at the program level, identifying patients due for review. PSP automatically creates updated verification records using existing data while flagging fields for revalidation.
After these records are created, the program lead assigns them to a patient services rep, who takes over patient-specific outreach and verification.
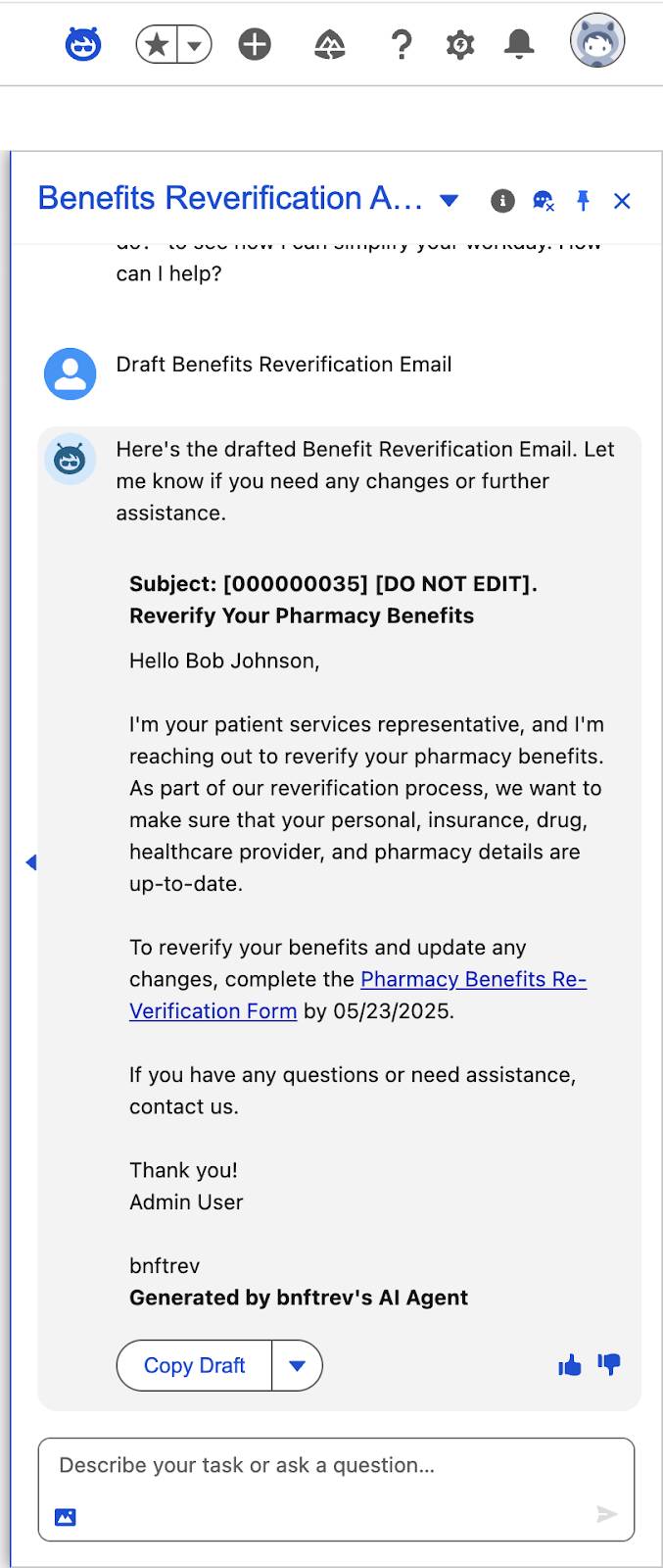
Lief Hansen receives his assigned cases and selects Lisa’s record from the Reverification List.
On her Care Benefit Verification Request (CBVR) record, Agentforce suggests the next best action, which is to generate an outreach email to confirm whether her insurance has changed.
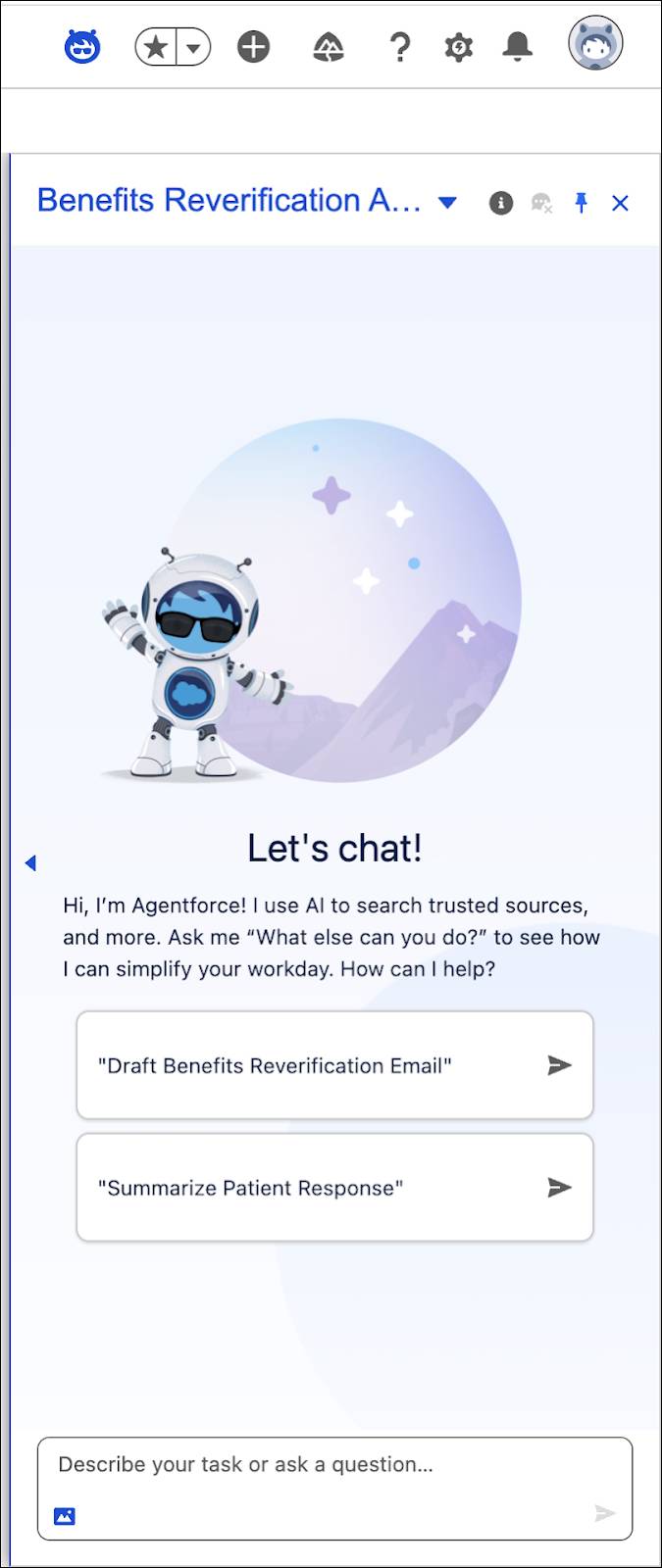
Lief sends the email directly from Lisa’s record, triggering the patient confirmation process.
The next day, Lisa completes the reverification form, and Agentforce instantly summarizes her response. If no updates are reported, her benefits are confirmed. If her insurance has changed, Agentforce helps Lief issue a new verification request.
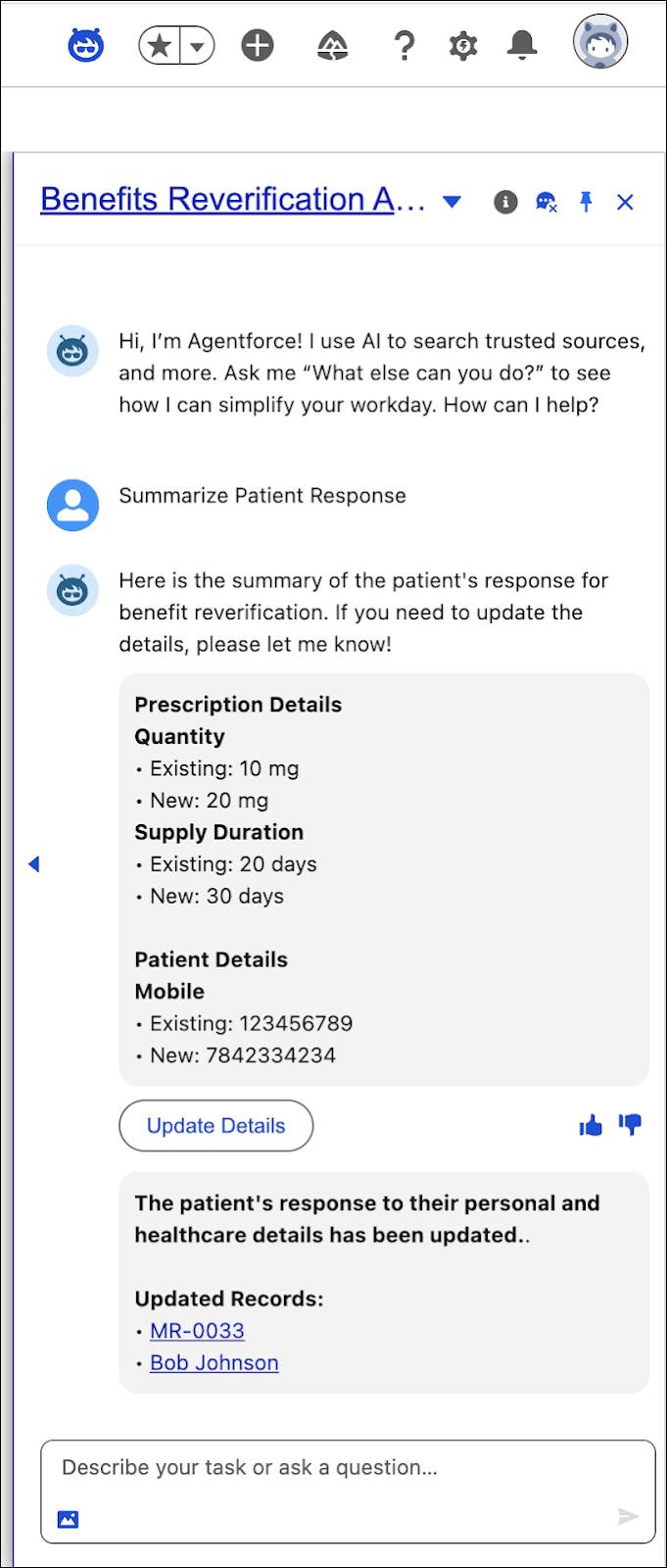
If payer follow-up is required, Agentforce generates a structured call script. After that, Lisa’s benefits record is updated, and a new Benefits Summary is generated, providing clarity for both her and her provider.
Lisa’s story shows how PSP for Life Sciences Cloud makes verification and reverification smoother with automation and AI. With accurate, up-to-date coverage information, Lisa can confidently continue her treatment without unexpected delays, while PSRs like Lief can shift their focus to proactive patient support instead of manual verifications.
Now that Lisa’s benefits are confirmed, she’s ready for the next step: enrolling in a financial assistance program to help manage out-of-pocket costs and ensure treatment continuity.