Enhance Patient Services
Learning Objectives
After completing this unit, you’ll be able to:
- Explain how Agentforce improves operational efficiency in Patient Services Programs.
- Describe how patient services reps use Agentforce to accelerate pharmacy benefits reverification.
- Identify how prebuilt agent skills reduce manual effort and improve program outcomes.
Navigate the Path to Patient Care
For a patient starting a new therapy, the path from prescription to treatment is rarely a straight line. It’s a journey filled with logistical hurdles including insurance approvals, prior authorizations, and pharmacy onboarding. The patient services program (PSP) rep is the essential guide for this journey, the liaison who ensures every step is completed correctly and on time.
But this role is often bogged down by administrative drag. Reps spend their days navigating a labyrinth of manual tasks, including rechecking benefits, interpreting insurance responses, and collating patient updates. This friction doesn't just slow down the rep, it delays patient care.
Agentforce for Patient Services acts as an intelligent partner, embedding digital labor directly into Life Sciences Cloud. It automates the routine logistics and surfaces critical insights, clearing the path so your team can focus on what truly matters: guiding the patient.
In this unit, you follow one of the most common workflows—Pharmacy Benefits Reverification—to see how the agent handles a complex, multi-step process with precision and speed. Then you explore other ways Agentforce boosts patient support.
Draft the Request
Meet Sarah, a PSP rep for a new migraine therapy. A Care Benefits Verify request lands on her worklist for an existing patient whose insurance details need reverification. This is a critical point in the process. Traditionally, it meant a manual assembly of data: tracking down the relevant fields, composing an email, and carefully inserting the correct links.
With Agentforce, the handoff is flawless. Sarah simply prompts the agent, “Draft Benefits Reverification Email.”
In seconds, the agent composes a ready-to-send communication. It intelligently gathers the necessary information—the patient’s name, the prescribed drug, and a secure link for them to update their information—and assembles it into a perfectly formatted email.
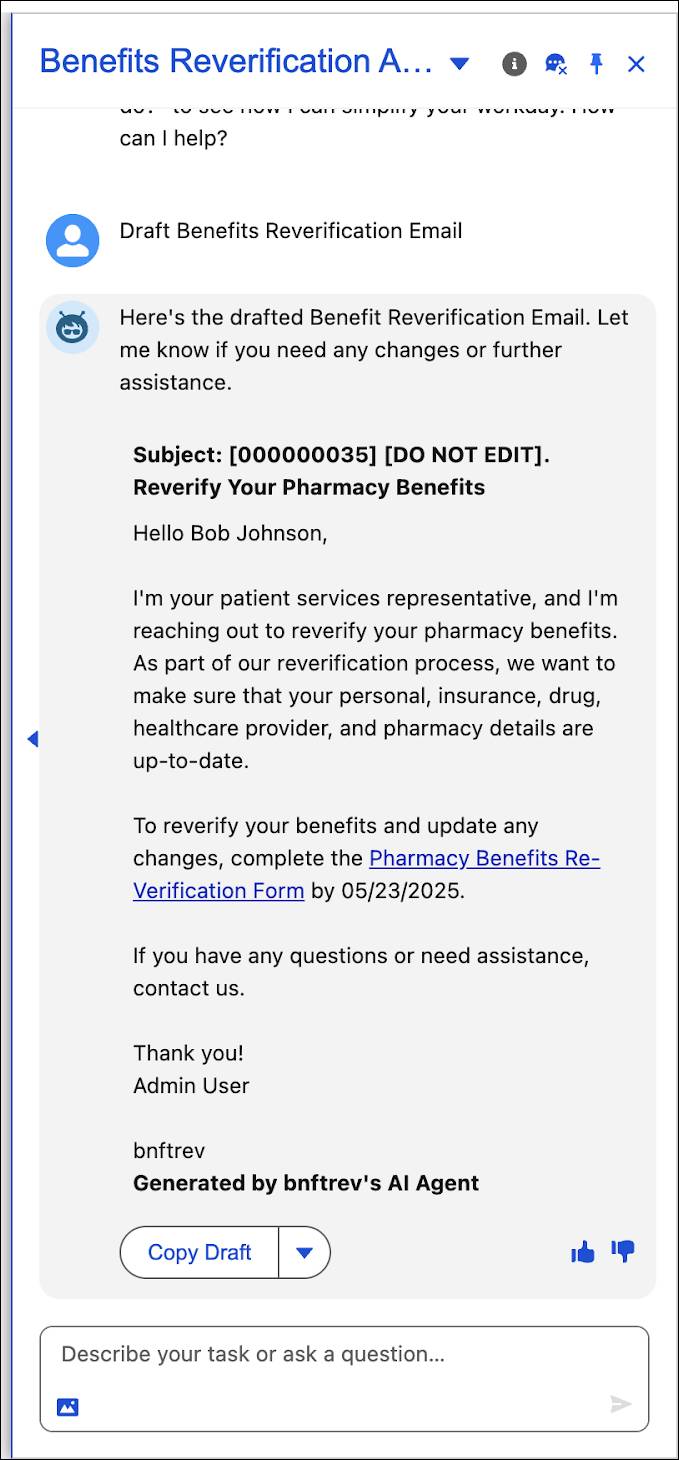
Sarah gives the draft a quick review and sends it directly from the console. The moment it’s sent, the system status flips to Pending Confirmation. The process is moving, with zero chance of error.
Summarize the Response
A few hours later, the patient submits their updated information. The system automatically updates the status to Received Confirmation, and now Sarah asks one thing: what’s changed?
She doesn’t compare the two records. She simply asks the agent to summarize the patient’s response.
This triggers an intelligent comparison. The agent goes beyond summarizing the new information to generate a concise briefing that highlights only the changes, which includes in this case, an updated insurance ID and a new preferred pharmacy. It distills the extraneous details, giving Sarah a clear, immediate picture of what's new without making her guess or navigate multiple tabs.
Update Records with Guardrails
With a clear understanding of the updates, Sarah is ready to sync the patient’s records. For routine changes such as a new address or pharmacy, the agent presents a simple Update Details button. One click, and the records are updated.

But the agent is also programmed with the relevant protocols. It recognizes that a change in insurance details is a critical event that requires human validation. In this scenario, the one-click update button doesn’t appear. Instead, Sarah is guided to manually create a new insurance record, ensuring a proper audit trail is created.
This thoughtful blend of automation and oversight respects the built-in guardrails of regulatory compliance.
Thanks to Agentforce, Sarah has completed a complex workflow in minutes, not hours, with full traceability and the confidence that comes from having an intelligent and protocol-aware partner.
Now check out some of the other ways Agentforce simplifies the work of PSP teams.
Discover Additional Agentforce Features for PSP Teams
Benefits reverification is just one way Agentforce helps PSP teams work smarter. The agent's ability to act on complex business logic brings a new level of intelligence to other high-volume, content-intensive tasks.
Verify Pharmacy Benefits
The first phone call to a new patient is a high-stakes moment that sets the tone for their entire journey. Agentforce transforms this critical first touchpoint from a cold call into a prepared, professional consultation. It does this by acting as both an expert scriptwriter and a meticulous scribe.
-
As the scriptwriter: Before the call, the agent scans the patient’s record to see what information is missing. It then generates a dynamic call script with a numbered list of targeted questions designed to fill those specific gaps. Instead of a generic script, your rep gets a personalized conversational guide, ensuring they capture every required detail on the first try.
-
As the scribe: After the call, the agent takes the newly gathered data and instantly composes a professional structured benefit summary. It follows a complex set of rules to format dates, translate technical insurance terms into plain language, calculate financial details, and embed required legal disclaimers, producing a clear, compliant document in no time.
Summarize Intelligent Outcomes
Patient services programs are measured by results. But sifting through spreadsheets of performance data to find the story—to understand what's working, what isn't, and what's missing—is a time-consuming, manual effort.
Agentforce steps in as your on-demand analyst, generating sophisticated outcome summaries at both the individual patient and aggregate program levels. When a program lead requests a summary, the agent conducts an analysis in three distinct steps.
-
First, it triages the data. The agent intelligently sorts every performance indicator into clear, intuitive categories, separating positive trends from areas of concern and flagging any critical data gaps. This initial sort provides an immediate, high-level understanding of program health.
-
Next, it builds a narrative. For outcomes that are off-track, the agent doesn’t just state the problem, it frames it with a solution. It quantifies the decline and then surfaces specific, data-driven recommendations such as Set Up Call with Patient to help the team get back on course. What’s more, it highlights what’s working, providing clear evidence of program wins.
-
Finally, it delivers a clean report. The agent smartly handles conditional logic, omitting irrelevant data. This ensures that the final summary is focused, uncluttered, and immediately actionable.
By embedding this analytical logic directly into the workflow, Agentforce transforms mountains of raw data into strategic insight, helping teams understand program effectiveness and take immediate, targeted action to improve patient outcomes.
From Paperwork to Patient Connection
In this unit, you saw Agentforce step into the role of the ultimate patient services partner. It manages the entire benefits reverification loop, from composing contextual outreach, to providing the essential briefing on what changed, and finally, updating the records with a single, protocol-aware click.
You also saw it take on other roles, such as an expert scriptwriter for those critical first calls and a sharp analyst that turns raw outcome data into strategic, actionable reports.
The result is an intelligent partnership. The agent masters the complex logistics so your team can focus on the human connection at the heart of patient care.
In the next unit, the focus shifts from the patient's journey to the provider relationship. See how Agentforce empowers commercial and medical teams to plan and execute more effective interactions.