Onboard New Providers and Ensure Ongoing Success
Learning Objectives
After completing this unit, you’ll be able to:
- Describe the key steps of onboarding and ongoing support.
- Explain how to provide ongoing support.
Provider Onboarding
Once the provider contract is signed, payers must pave the way for provider success through a personalized and effective onboarding program. The exact onboarding steps and actions may vary based on the attributes of the payer. Initiating a go-live program in the same system as the full provider onboarding journey makes handling those dynamic decisions efficient.
Although the specifics often vary, there are some common steps we can look at more broadly. Here are the key steps of provider onboarding.
- Integrate data.
- Assign coordinator.
- Activate provider portal.
- Provide training and enablement.
And here’s a summary of each step.
Step |
Summary |
|---|---|
Integrate data. |
Automatically route the appropriate data to the appropriate downstream systems. For example, deliver provider reimbursement terms to the claims system. |
Assign coordinator. |
Assign the appropriate provider coordinator based on provider characteristics and other factors. |
Activate provider portal. |
Provide a central portal that has all key actions and communication needed to complete the onboarding and perform other key tasks. |
Provide training and enablement. |
Deliver effective training and enablement on key processes and practices. |
Ongoing Provider Support
After the onboarding of new providers, health plans must continue to deliver solutions to ensure their ongoing success.
Here are the key steps of ongoing provider support.
- Configure automated reminders.
- Enable claims services.
- Embed live chat.
- Provide support and resolution.

And here’s a summary of each step.
Step |
Summary |
|---|---|
Configure automated reminders. |
Deliver automated reminders to providers via their preferred channel of communication. For example, send reminders about actions needed around contract renewal and recredentialing. |
Enable claims service. |
Support integrations to facilitate claims display and intake in a provider portal. |
Embed live chat. |
Embed live chat in a provider portal, and give providers the chance to resolve issues in a snap. |
Provide support and resolution. |
Use case management and routing tools to initiate, manage, and resolve all cases faced by providers. |
Let’s check back in with Cumulus Health Plans and see how it uses an assortment of Salesforce tools to onboard and provide ongoing support for Dr. Zamadi and her team.
Set Up for Success
After the contract is signed, Cumulus Health Plans makes sure to set up providers for lasting, ongoing success. To enable various welcoming activities, Cumulus relies on a number of Salesforce tools. And it’s not only the provider (Dr. Zamadi) that needs onboarding, but also the provider office team who handle key tasks such as scheduling, billing, and claims.
Broadly, the Cumulus onboarding experience falls into the following two categories.
- Set up integrations for communicating with the provider’s downstream systems that handle key processes like claims.
- Deliver training and communication to the provider and team to ensure they can successfully complete all key tasks.
In this section, we focus more on the second category, since the specific integrations needed for different organizations can vary greatly.
Let’s check in with Colin Sparks, the provider specialist assigned to Dr. Zamadi’s case.

Just like the other specialists at Cumulus, Colin has his own personalized Go Live Specialist Home page where he can easily access his queue and perform other key onboarding actions.
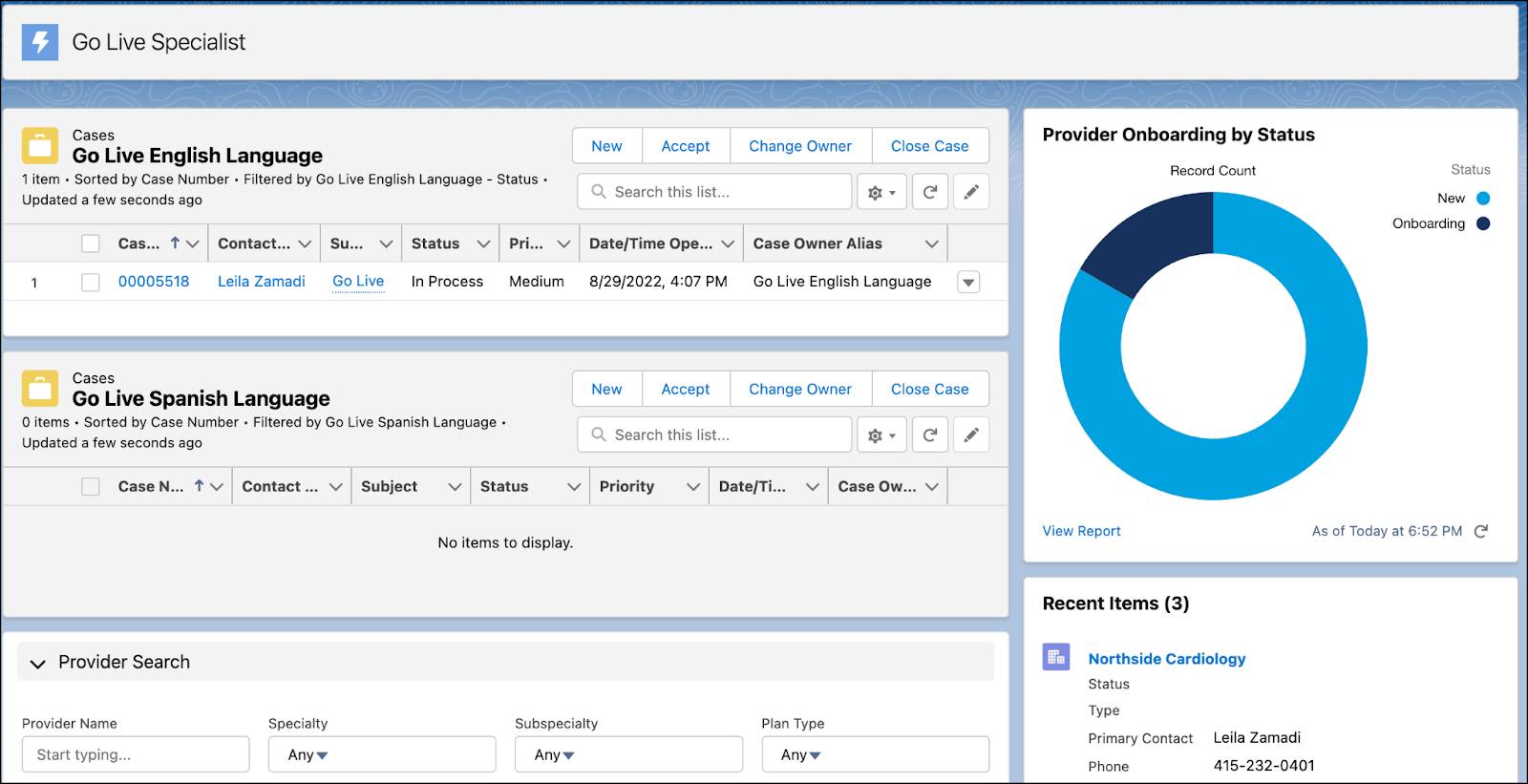
Colin starts his day by diving into Dr. Zamadi’s Go Live case record. Conveniently, the work guide is waiting for him with a list of onboarding tasks to complete.

In a real implementation, the list of onboarding steps can be much longer. The key thing to note is how flexibly the Flow Orchestration and case management tools meet different needs across all stages, while giving all users an integrated experience.
To further support new providers, health plans can easily set up a variety of resources on the provider portal.
Over the next week, Dr. Zamadi and her team regularly visit the portal to complete the training, which is delivered via enablement sites. Enablement sites deliver unique learning content through a branded experience. Searchable FAQs, documentation, and knowledge articles provide additional information. And thanks to embedded chat, her team can reach out and receive more advanced in-context support whenever they need it.
In a short time, Dr. Zamadi and her team receive all the tools and training they need to effectively participate in the network.
Let’s flash-forward one month. Dr. Zamadi and her team are pleased with how smoothly things are going. They regularly receive automated reminders about key actions and events that need to be completed. For example, Dr. Zamadi receives a reminder via a secure message that Colin will be visiting the office to check in personally on how things are going. And the appointment is automatically added to her calendar on the portal.
Everyone on Dr. Zamadi’s team knows exactly what to do when they run into issues and feel supported every step of the way. Just last week, they had a question about a claim reimbursement. The provider portal enables fast, in-context communication so they initiate a chat for the claims inquiry.
When the chat is received, it automatically routes to a queue specialized in handling such provider inquiries. The support agent who takes on the inquiry is empowered with access to real-time data via integration, contract terms for Dr. Zamadi, and knowledge article recommendations. Together, they are able to resolve the question in a few minutes.
Dr. Leila Zamadi and her team now have a lot more time to focus on patient care. And Cumulus has total confidence in its provider data, actionable insights, and single system of engagement. It’s truly a win-win-win for payers, providers, and members alike!
Resources
- Salesforce Help: Enablement Sites (myTrailhead)
- Trailhead: Build an Experience Cloud Site with Knowledge and Enhanced Chat