Identify and Recruit Your Network
Learning Objectives
After completing this unit, you’ll be able to:
- List the main steps of the provider recruitment process.
- Explain how Provider Network Management helps the recruitment team at each step.
- Explain how each user participates in the recruitment process.
Provider Recruitment Steps
You may have heard this before, but a health plan is only as good as the quality and depth of the providers it can attract. So the effective recruitment of providers is the critical first stage in building a strong provider network.
For a provider network to be successful, the recruitment team must have tools to:
- Analyze its existing network.
- Identify network gaps.
- Develop campaigns to attract top providers.
- Build personalized workflows and interactions to support the application process.
Here are the main steps that the recruitment team must take to recruit providers.
- Target new providers.
- Submit provider request.
- View provider leads.
- Segment and assign leads.
- Review leads.

Provider Network Management offers a variety of resources to support payers across every step of the recruitment process. Let’s find out how Provider Network Management helps recruiters at each step.
Step |
How Provider Network Management Helps |
|---|---|
Target new providers. |
To build a robust and effective network, health plans need to identify high-value candidates to bring into the network. Using CRM Analytics, recruiters can use dynamic analytics tools to set specific criteria, evaluate network adequacy, and identify high-value providers. |
Submit provider request. |
The opportunity for network growth also happens organically. An inbound provider request involves a provider who reaches out directly to a health plan about becoming a participating provider. To make this request simple and quick for the provider, Provider Network Management provides guided workflows that launch from a payer portal or website. |
View provider leads. |
Provider leads come from a variety of sources: hospital systems, list purchases, competitive analysis, and more. Regardless of the source, Provider Network Management enables the recruiting team to view and manage their provider leads in a single place. |
Segment and assign leads. |
Using embedded analytics tools, the recruitment team segments their provider lead lists across various characteristics such as geography, type, and specialty. Lead assignment and skill-based routing rules then assign the leads to the appropriate recruitment specialist. |
Review leads. |
With lead management and CRM Analytics, recruiting specialists can review assigned leads and identify any missing information. Then, thanks to dynamic workflows, the assigned specialist can reach out to the provider and collect any missing information. The data collected can then trigger automated workflow rules that progress the provider into the credentialing stage. |
To take a closer look at these steps, let’s return to Cumulus Health Plans and see how its team uses an assortment of Salesforce tools to recruit the best and brightest payers to its health plan network.
Find the Right Providers
Let’s check back in with Greg Lawson, the provider network director at Cumulus. His job is to identify the right providers to recruit into the network.

Greg examines the network adequacy data, identifying ways to strengthen the provider network. He pulls up his Provider Network Adequacy dashboard, which the implementation team has built out.
The dashboard, powered by CRM Analytics, is configured so Greg can easily filter by state and practitioner type to receive instant graphs and visualization on the percentage of patients who can access practitioner types within a designated distance limit. These filters serve only as an example. Health plans can add additional layers and data sources to enable more granular analysis.
Greg sets filters and looks at the data for General Practice providers in Massachusetts.
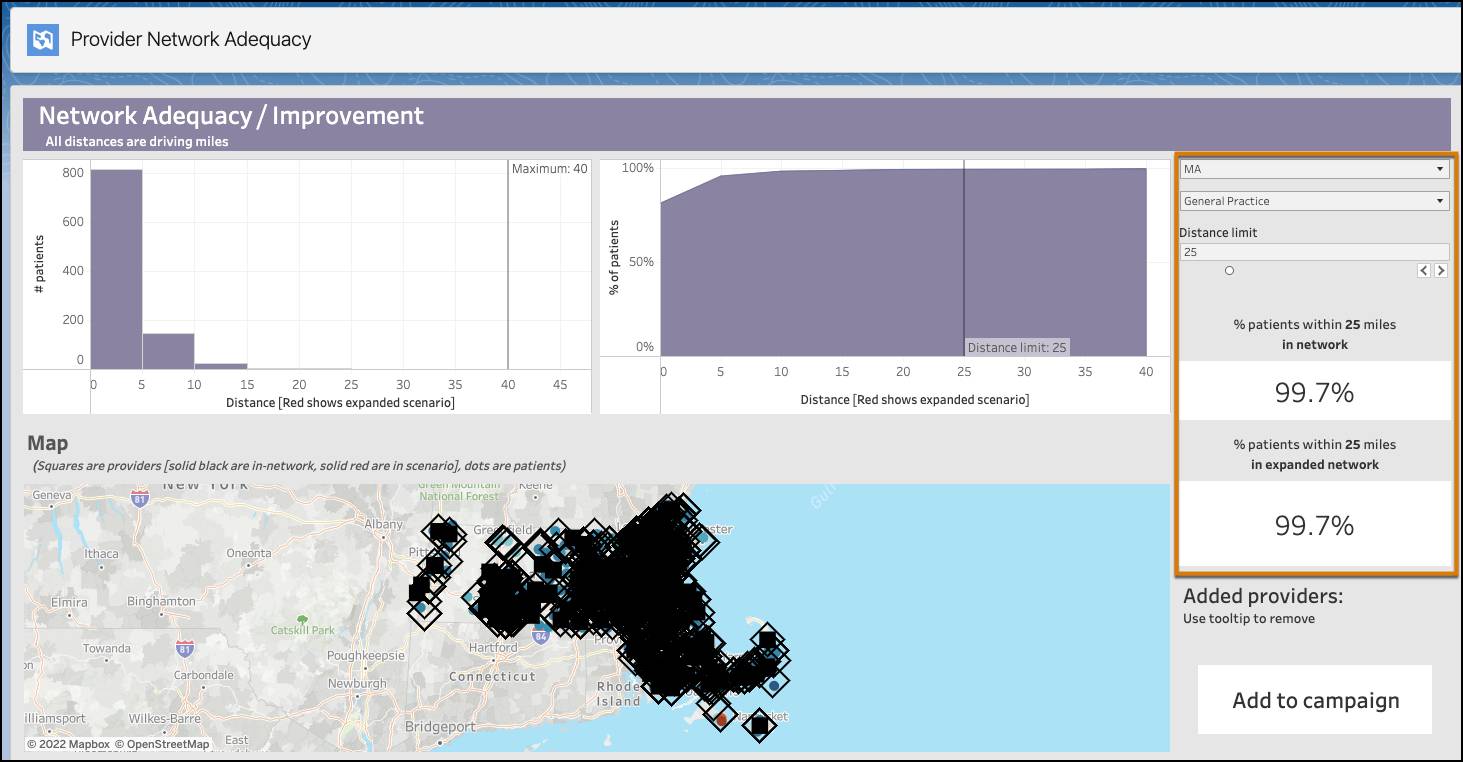
He discovers that 99.7% of patients can access a general practice provider within 25 miles of their home address, not too bad!
Next, he sets the filters to analyze the adequacy metrics for Physical Medicine in Massachusetts.
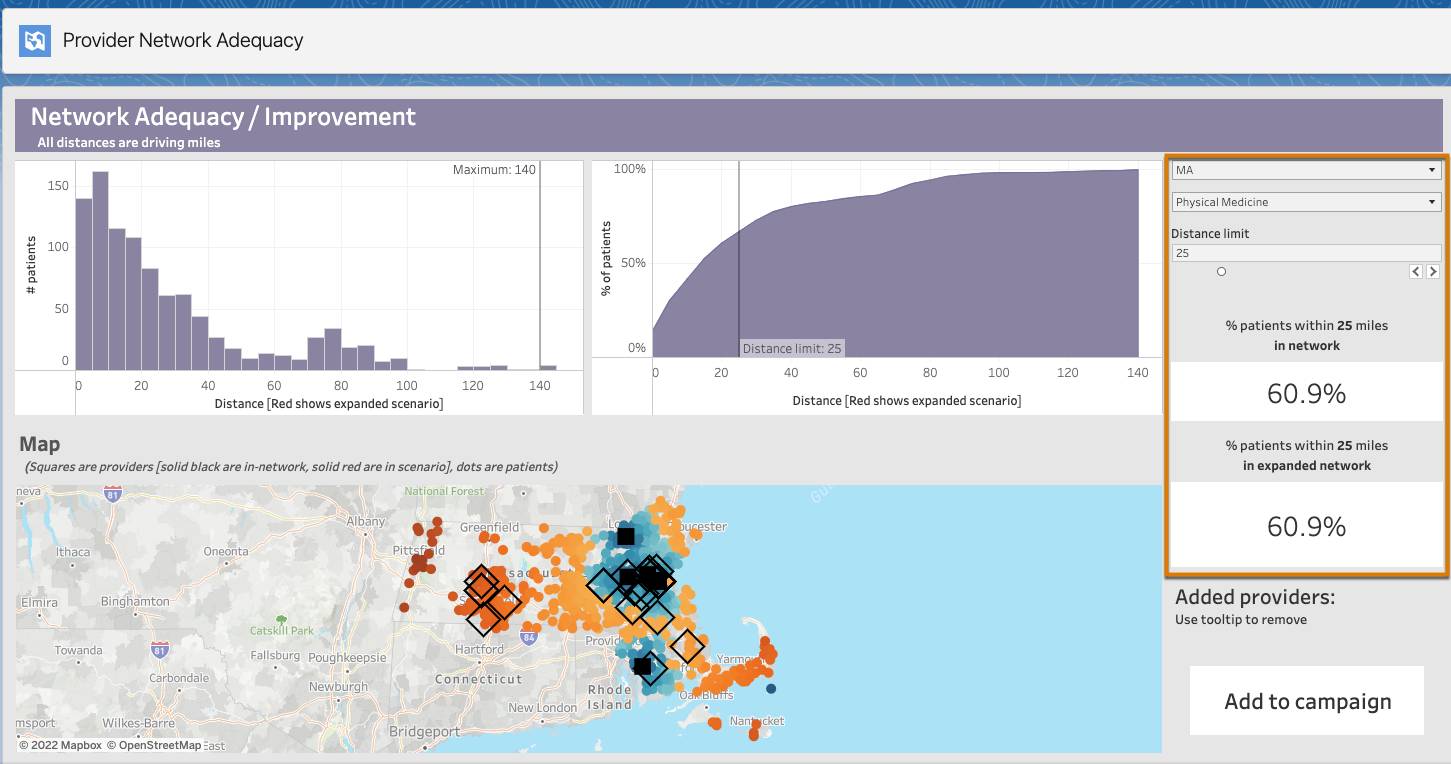
For this specialty, Greg observes some major gaps, with only 60.9% of patients able to access a physical medicine provider within 25 miles.
Greg takes a closer look at the map to better understand where these gaps exist and to identify potential candidates to fill them.

The map color codes the members to illustrate their proximity to a physical medicine provider. Members in dark blue are closest to the provider specialty, while those in dark red are the furthest away from the provider specialty.
The map also captures in-network and out-of-network providers. The in-network providers are represented by the filled-in squares. Those providers who are not a part of the network are represented by the outlined diamonds.
Aware that members in western Massachusetts have limited access to this specialty, Greg looks more closely at these prospective providers.
Greg first checks Peggie Zbonack, a provider located just south of Springfield, Massachusetts.

Greg sees that Dr. Zboncak has both a high-quality score and a high propensity to join. He initiates a forecast by clicking Add to network. Immediately, Greg sees how the adequacy data changes if Dr. Zboncak joins the network. Simply by adding this single provider, the adequacy metric increases by over 7%.

Greg continues to analyze the adequacy data. He adds multiple providers and determines the highest value recruitment candidates across different areas and specialities.
Target New Providers
Once Greg has a list of desirable provider candidates, there are multiple next steps he can take. For one, he could reach out directly to each provider, creating a one-off task in which he sends out a personalized email. Or he could assign them a dedicated recruiting specialist who could reach out to them on a manual but recurring basis.
Best of all, though, Greg can assign these providers to a campaign. A campaign is a simple way to manage and automate complex marketing plans and assets in a single journey. Configure different campaigns for different initiatives and then add providers to the appropriate one.
Cindy Singh, the marketing and recruiting coordinator at Cumulus, is in charge of Cumulus’s campaigns. Using Marketing Cloud Engagement’s Journey Builder, Cindy sets up a number of campaigns for different purposes. For provider recruitment, Cindy configures a specific journey that automates provider engagement.
After reviewing Dr. Zamadi’s information, she adds her to this campaign. Dr. Zamadi is a highly regarded cardiologist who checks off a number of geographic and specialization boxes.
Cindy has designed this campaign to respond to different contingencies, with personalized paths for different provider specialties.

Automating key moments in the recruitment process allows payer organizations to efficiently scale without overburdening the recruitment team with a heavy volume of repetitive tasks. It frees the team up to focus their time and effort on more personalized communication. And they can analyze the effectiveness of campaigns to make continual improvements. Pretty powerful stuff.
Submit Provider Requests
In addition to all the outbound tools for identifying and targeting high-value providers, Cumulus allows providers to reach out and express interest in joining the network.
Such inbound requests are called “push” requests, in contrast to the “pull” model, which involves more active recruitment by the provider.
To support this self-service model, Cumulus invites providers to submit a provider registration application. The implementation team at Cumulus builds this application using OmniStudio tools such as OmniScript. Then, the team embeds the flow in Cumulus’s provider portal.
Following the campaign email link, Dr. Zamadi submits a provider registration request on the provider portal.

Dr. Zamadi enters basic details about her practice and then receives confirmation.

Behind the scenes, the OmniScript generates a lead record from the provided data.
View All Leads in One Place
New provider information comes to Cumulus from a host of sources, such as hospital systems, list purchases, competitive analysis, and inbound requests like Dr. Zamadi’s. Regardless of the source, the provider recruiting team can review all their provider leads in one place.
They use the Provider Recruiting dashboard to segment and analyze leads across key metrics, such as source, specialty, campaign, and date. The dashboard gives recruitment specialists dynamic visualizations into prospective providers.
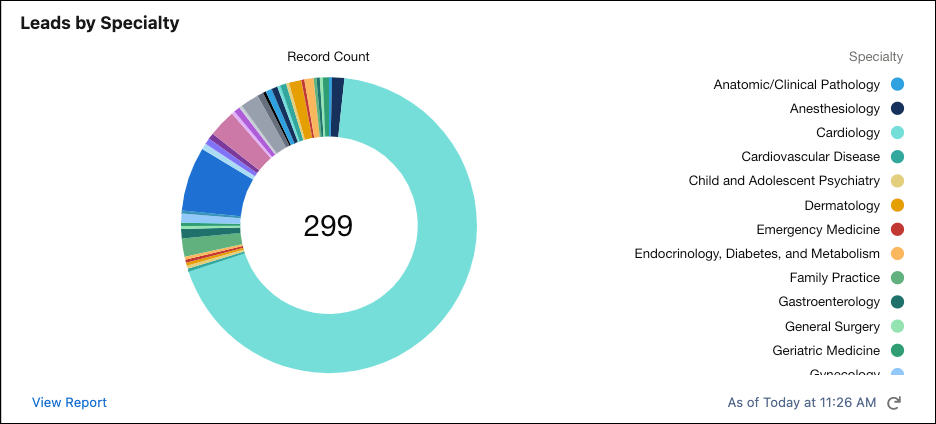
By clicking View Report, users can generate a customized report across a variety of filters. And the recruitment team can further customize the dashboards to meet business needs.
Assign Leads to the Right Resource
Providers come in all shapes and sizes–hospitals, group practices, individual practitioners–and it’s important for recruitment teams to have a strategy to assign the appropriate recruiting resource.
Using CRM Analytics, the Cumulus recruiting team segment provider leads in a number of ways. They then use automation rules to assign the segmented leads to the appropriate recruiting specialists based on provider characteristics such as geography, type, and specialty.
Based on her speciality and location, Dr. Zamadi is assigned to the recruiting specialist Cindy Singh. On her provider recruiting dashboard, Cindy reviews her Assigned Leads queue, where Dr. Zamadi is at the top of the list.

Cindy is now ready to take a closer look.
Review Leads and Move to the Next Stage
After receiving notification of the new provider lead assignment, Cindy visits Dr. Zamadi’s lead record page. It contains information captured from the registration and Einstein Discovery forecasts that predict Dr. Zamadi’s likelihood to join the network.

Cindy quickly notices that some key information is missing, such as Dr. Zamadi’s National Provider Id (NPI).
Conveniently, Cindy performs key actions straight from the record page. Using phone system integration, Cindy calls Dr. Leila Zamadi from the lead page. A call script launches and helps Cindy collect the missing information.

After the call, Cindy has all the information she needs to move Dr. Zamadi onto the credentialing stage, which we explore in the next unit.
Resources
- Salesforce Help: Provide Patient and Member Insights with Analytics
- Salesforce Help: Campaigns
- Trailhead: Journey Builder Basics
- Trailhead: Build and Administer CRM Analytics