Get Started with Provider Management
Learning Objectives
After completing this unit, you’ll be able to:
- Describe common challenges associated with provider management.
- Explain how Provider Management simplifies managing service providers and referrals.
- Define the types of objects in the Provider Management data model.
Before You Start
Before you start this module, consider completing the following recommended content.
-
Benefit Management Data Model in Public Sector Solutions
-
Social Program Management Data Model in Public Sector Solutions
-
Admin Essentials for Public Sector Solutions
Provider Management in the Public Sector
Keeping a community healthy and happy is truly a team sport. That’s why government agencies join forces with healthcare professionals, counselors, trainers, and other specialists to alleviate various problems that constituents experience.

In the Benefit Management Data Model in Public Sector Solutions and Social Program Management Data Model in Public Sector Solutions modules, you learn how government agencies use Public Sector Solutions to manage cases, develop personalized care plans, and deliver certain types of benefits. However, constituents often require services that fall outside of the purview of the government.
In situations like these, caseworkers coordinate with providers who specialize in specific types of aid. These specialties include healthcare, child and senior welfare, employment services, judicial management, financial assistance, and more.
Referrals and Service Monitoring
Caseworkers have lots of day-to-day responsibilities, including referring constituents to service providers and monitoring the constituent experience. Let’s dig a little deeper into the process.
While working on a case, a caseworker assigns goals and benefits to a constituent to help them overcome certain challenges. If the constituent’s issue calls for outside expertise, the caseworker connects them to a specialized provider using a referral. Referrals have information about the constituent, their issue, and other important details.
Here’s a typical provider referral process.
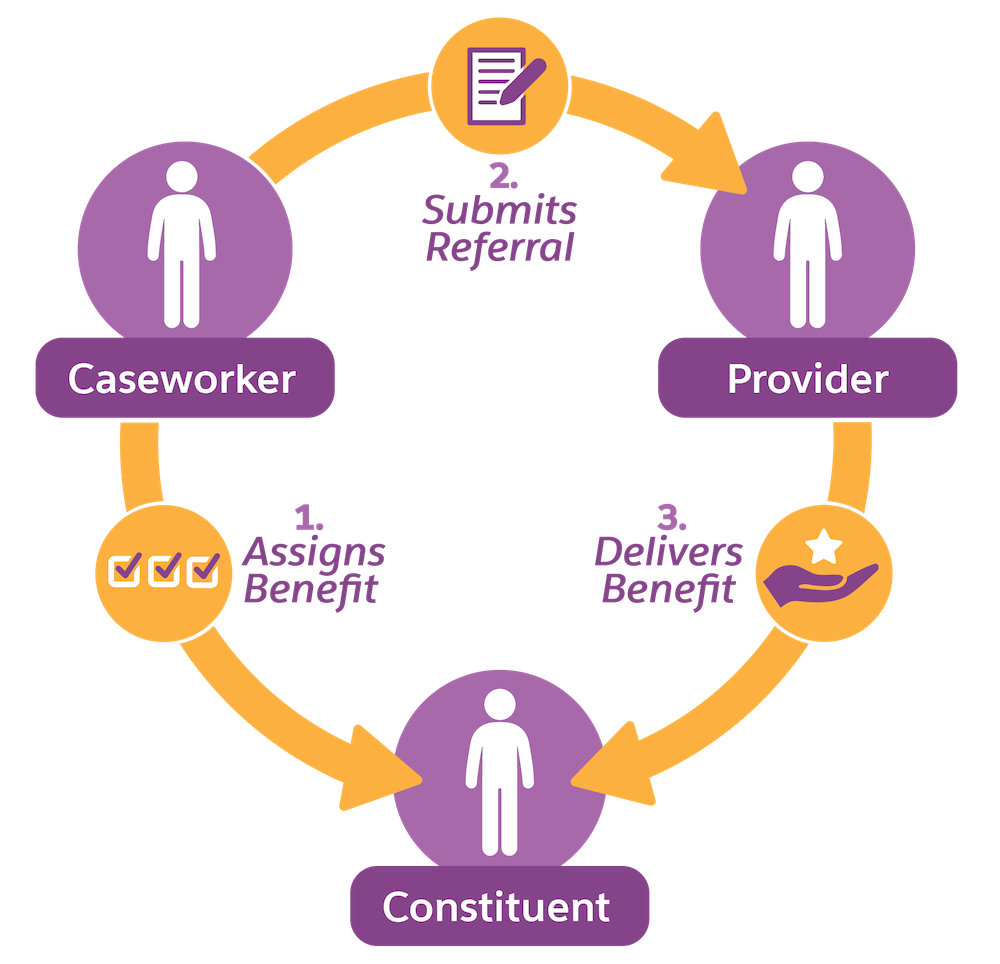
The provider reviews the referral, determines whether they have the right resources to provide the service, and either accepts or declines the request. If the provider accepts the referral, they start providing service to the constituent, sharing progress updates with the caseworker until the service lifecycle is complete. Caseworkers rely on these updates to ensure that the constituent receives the prescribed benefits and that they’re progressing toward their goals. Agencies use this knowledge to track the advancement of a case or care plan, report on the effectiveness of each provider, and make timely payments to the provider for their services.
Common Challenges
As with all forms of collaboration, trust, communication, and efficiency are vital. Agencies must identify service providers that are qualified, reliable, and meet strict regulatory requirements, and then set up clear lines of communication for the referral process. Caseworkers must navigate the unique combination of specialties, facilities, and availability of each provider, and then collect and transmit all the required constituent information to begin care.
Unfortunately, this workflow is fraught with challenges.
Tishon, the Salesforce Admin for the City of Cosville, regularly meets with the Department of Public Services caseworkers to discuss process improvements and to collect feedback.

Here are some of the recurring roadblocks that caseworkers report.
- Caseworkers rely on phone calls and emails to manually collect all of the necessary data to recruit, vet, and onboard new providers, which is time consuming.
- To identify the right provider to deliver a benefit, caseworkers must sift through several spreadsheets of provider data, which often contain inconsistent or outdated information.
- When creating referrals, caseworkers must painstakingly track down and copy over constituent information into an email to the intended provider.
- Providers often fail to report service delivery to the agency, so caseworkers can’t check on constituent progress or arrange timely and accurate payments to the provider.
- Without a way for caseworkers to verify provider credentials and record feedback, constituents might encounter poor conditions at provider facilities, uncredentialed staff, or other quality issues that degrade their experience.
Tishon knows this level of service won’t fly in Cosville. That’s why she’s so excited to hear about Provider Management with Public Sector Solutions.
Provider Management Features
Provider Management strengthens the agency-provider partnership with increased transparency, flexibility, and efficiency. Scale up and manage your provider network, help caseworkers pinpoint the right provider faster, and monitor end-to-end service to ensure successful outcomes for constituents and timely payments to providers. Provider Management works alongside Social Program Management and Benefit Management objects in Public Sector Solutions.
Here’s a rundown of the features.
Provider Data
Collect essential data about each provider to build a comprehensive network without the countless phone calls and emails. Record information about specialties, facilities, operating hours, and schedules. Track individual practitioners associated with each provider, along with their credentials, education, and employment history. With a strong network of providers, agencies can route constituents to the right solutions and address common issues in the community.
Provider Search
Say goodbye to spreadsheets! With advanced, configurable search tools, caseworkers can quickly identify the right provider to fulfill a benefit assignment and address unique constituent needs. Narrow down the network by entering relevant criteria, such as the intended benefit type, care specialty, or operating hours. Then, apply filters to refine the results, such as setting a limit on the distance of facilities from the constituent. Group and sort search results and perform actions, for instance, launch a Omniscript guided flow to create a referral directly from the search results.
You can even create and organize your own set of custom search configurations to meet the needs of your agency.
Accelerated Referrals
Instead of copying and pasting information into emails, use a guided flow to quickly share constituent information with providers during the referral process. Send contact details, case details, and document attachments directly from your org objects. Providers can view the referral data right from their online portal, accept or reject the request, and submit benefit schedules for agency review.
Service Monitoring
Keep a close eye on service delivery to ensure constituent progress and timely payments to the provider. Through the online portal, providers can collaborate with your agency on referrals and share progress updates for each constituent. This way, your agency can track the status of service delivery, including enrollment and attendance of benefit sessions, and submit payments soon after the provider completes the services. You can integrate these Provider Management capabilities into any of your existing Public Sector Solutions Experience Cloud site templates.
Provider Insights
Use the centralized provider data in your org to build an analytics dashboard for evaluating constituent outcomes, measuring the performance and utilization of each provider, and ensuring credentials are valid and up to date. Assess provider utilization and constituent feedback so that you can identify underperforming providers or those that are no longer suitable for your constituents.
Provider Management bridges the gap between government agencies and service providers. With a collaborative online portal, advanced search capabilities, and a single source of truth, you can swiftly connect constituents with the right services to improve their circumstances.
Provider Management Data Model
In this module, you dive into the different objects in the Provider Management data model, exploring examples to understand the purpose of each component.
The interactive table breaks down the data model into six categories of objects.
Tishon has listened to the team of caseworkers and embarks on a mission to bring Cosville’s referral process into the 21st century.
In the next unit, explore the data model and discover the objects that store valuable nuggets of data about your constituents and providers.