Learn About Utilization Management
Learning Objectives
After completing this unit, you’ll be able to:
- Explain how payers and providers use Utilization Management for Health Cloud to improve patient care management.
- Explain how Health Cloud solves the common challenges of utilization management.
Before You Start
Before you start this module, consider completing the following recommended content.
The Need for Effective Utilization Management
Healthcare organizations face an ongoing challenge of balancing effective care with increasing costs.
This reality requires payers to make countless decisions every day regarding the necessity of care and communicate those decisions to healthcare providers and members. It’s not just payers that bear the burden. In dealing with multiple payers, each with their own guidelines, providers also face substantial challenges and costs in seeking authorizations for care requests. This manual process, often filled with errors and exceptions, can delay the provision of patient care.
What if all the stakeholders actively participate before considering the actual treatment? This is where utilization management (UM) comes in. At its core, UM ensures that patients receive the right care, at the right time, for the appropriate duration, and in the right setting.
Traditionally, health plans have used UM to manage healthcare costs through case-by-case evaluation of the appropriateness of care before its delivery. Under the fee-for-service model that used to be the industry norm, UM has primarily served to cut costs.
Today, healthcare has moved toward value-based models, in which care providers are reimbursed on the quality of clinical outcomes, not just the quantity of services delivered. This focus on quality leads health organizations to now view UM through a more holistic lens. Increasingly, payers and providers alike leverage UM not only to manage costs, but also to ensure quality care and manage risk.
Enter Utilization Management for Health Cloud: It’s a combination of features that streamlines and digitizes every stage of the UM process.
The Utilization Management Lifecycle
The key stages of UM include Need Assessment, Authorization Submission, Intake Management, Clinical Review, and Decision and Communication. These stages work together to ensure the delivery of quality care for members.

This table introduces the goal of each stage.
Stage |
Goal |
|---|---|
Need Assessment |
Providers determine whether an authorization request is required for a specific medical service. |
Authorization Submission |
Providers submit a formal request to payers for authorization of medical care. |
Intake Management |
Payers conduct an administrative review of an authorization request and route it to the appropriate resource. |
Clinical Review |
Payers evaluate the medical necessity and appropriateness of the requested service. |
Decision and Communication |
Payers communicate the final approval or denial of the requested service to providers and members. |
By following these stages, healthcare organizations ensure that medical services are reviewed in a consistent and evidence-based manner. This helps to optimize patient care while controlling costs.
How Utilization Management Solves Key Challenges
With the key stages in mind, here’s a look at the common challenges in UM and how Health Cloud provides specific tools to solve them.
Need Assessment
When a patient visits a healthcare provider, the provider must update the patient information in an electronic health record (EHR). They must also check service and diagnosis codes against the payer’s specific policies, which is a time-consuming and error-prone process. Payer organizations must then dedicate extensive resources to addressing these queries.
The OmniScript process library provides a guided flow for conducting need assessment, which organizations can customize.
Providers can use the EHR connector MuleSoft Direct for Health Cloud to directly pull patient and clinical information, greatly simplifying the information gathering process.
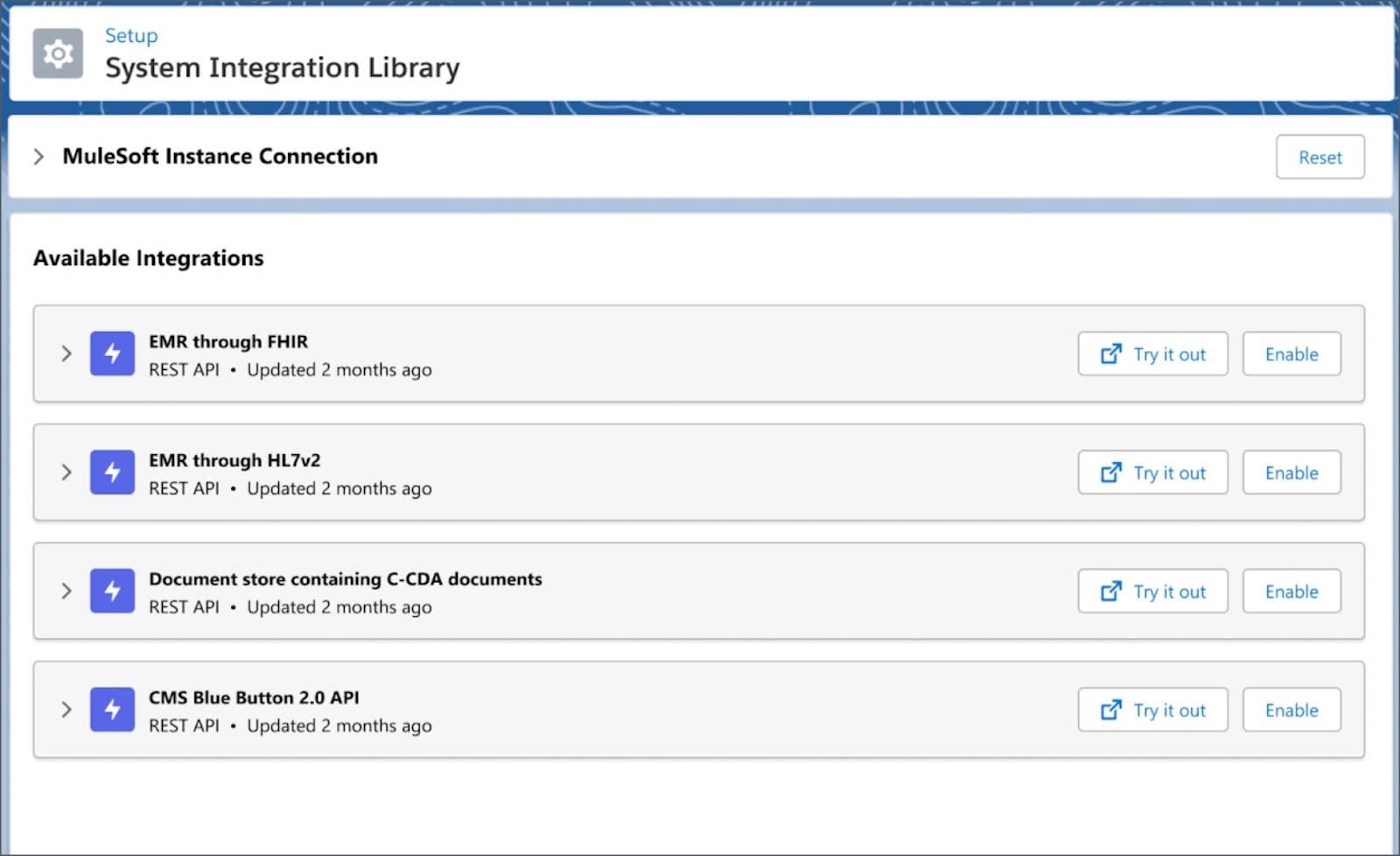
Using Business Rules Engine (BRE), payers can configure complex need assessment rules to further automate the process. They can extend these rules directly via Connect API or by setting up a provider portal using Experience Cloud.
Authorization Submission
Typically, the provider staff must make prior authorization (PA) requests via phone or fax, or must manually reenter patient and clinical data into the health plan’s portal.
Out-of-the-box guided flows enable fast, accurate, and digital submission of PA requests.
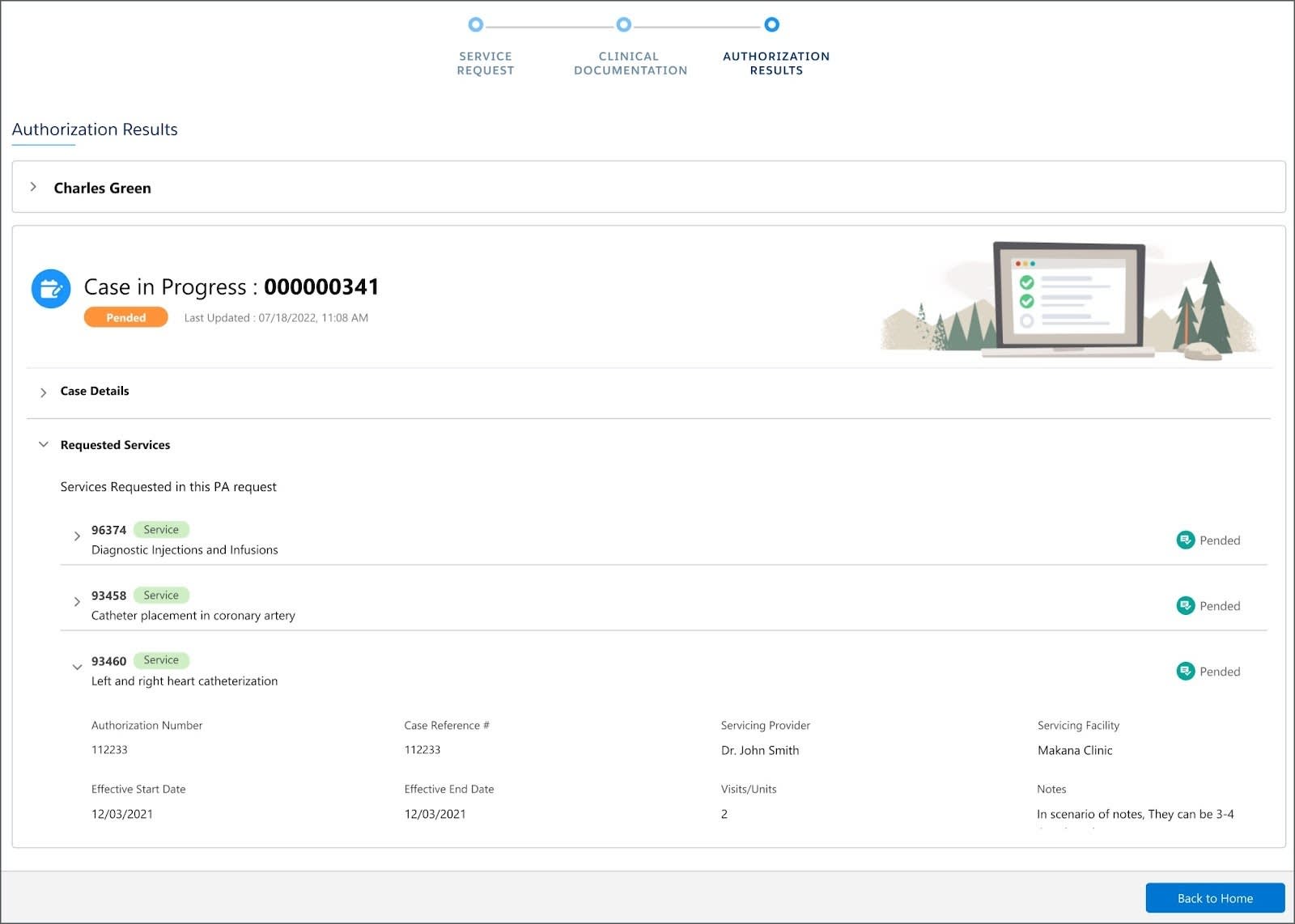
MuleSoft Direct for Health Cloud allows providers to easily pull patient and clinical information to quickly create authorization requests. Then, providers can submit the request electronically in a Da Vinci FHIR API format where it can be sent to the payer’s FHIR endpoint via Mule Connector.
BRE tools enable auto-approval conditions to be set for prescribed services. This leads to case deflection and a reduced burden on call center administrators and medical staff.
Intake Management
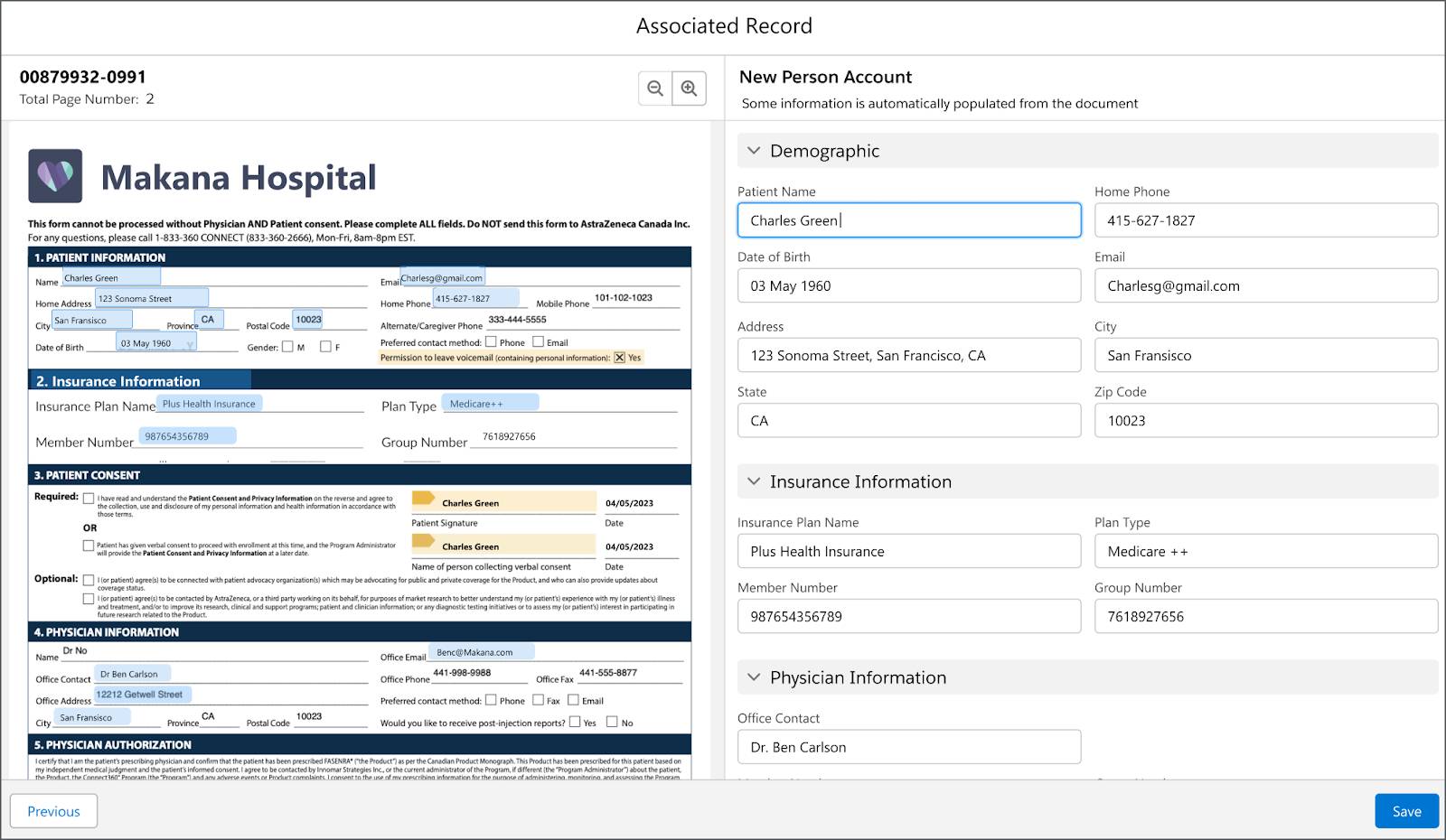
Due to interoperability challenges, intake specialists must manually enter requests into the UM application, and then review and route them for clinical review. Any errors in the request or data entry can cause delays and put the request on hold.
The specialist is also responsible for verifying eligibility and benefits, while ensuring that all necessary documents are attached to the request.
Health Cloud’s standards-based approach and integration tools make it easy to align authorization requests directly with EHR. Out-of-the-box Salesforce Healthcare APIs facilitate PA intake in Da Vinci FHIR R4 format.
Intake specialists can use Intelligent Document Automation (IDA) tools to process fax-based PA requests. And document checklists ensure all required documents are received with the initial request.
OmniChannel routing tools make it easy to configure rules for automatically assigning cases to the appropriate clinical resource. Queue-based routing (QBR) ensures authorization requests land in the right queue while skills-based routing (SBR) routes the request to the specialist with the required skills and capacity.
Clinical Review
UM clinicians don’t have an easy way to view medical necessity criteria, and must switch between different applications to gather necessary information. The clinicians often must request supporting documents from the provider, which is an offline process involving extensive coordination.
Health Cloud enables the integration of medical necessity criteria, improving the accuracy, consistency, and efficiency of clinician’s decisions.
The My Care Requests dashboard provides a centralized hub to view, prioritize, and take action on all active care requests.
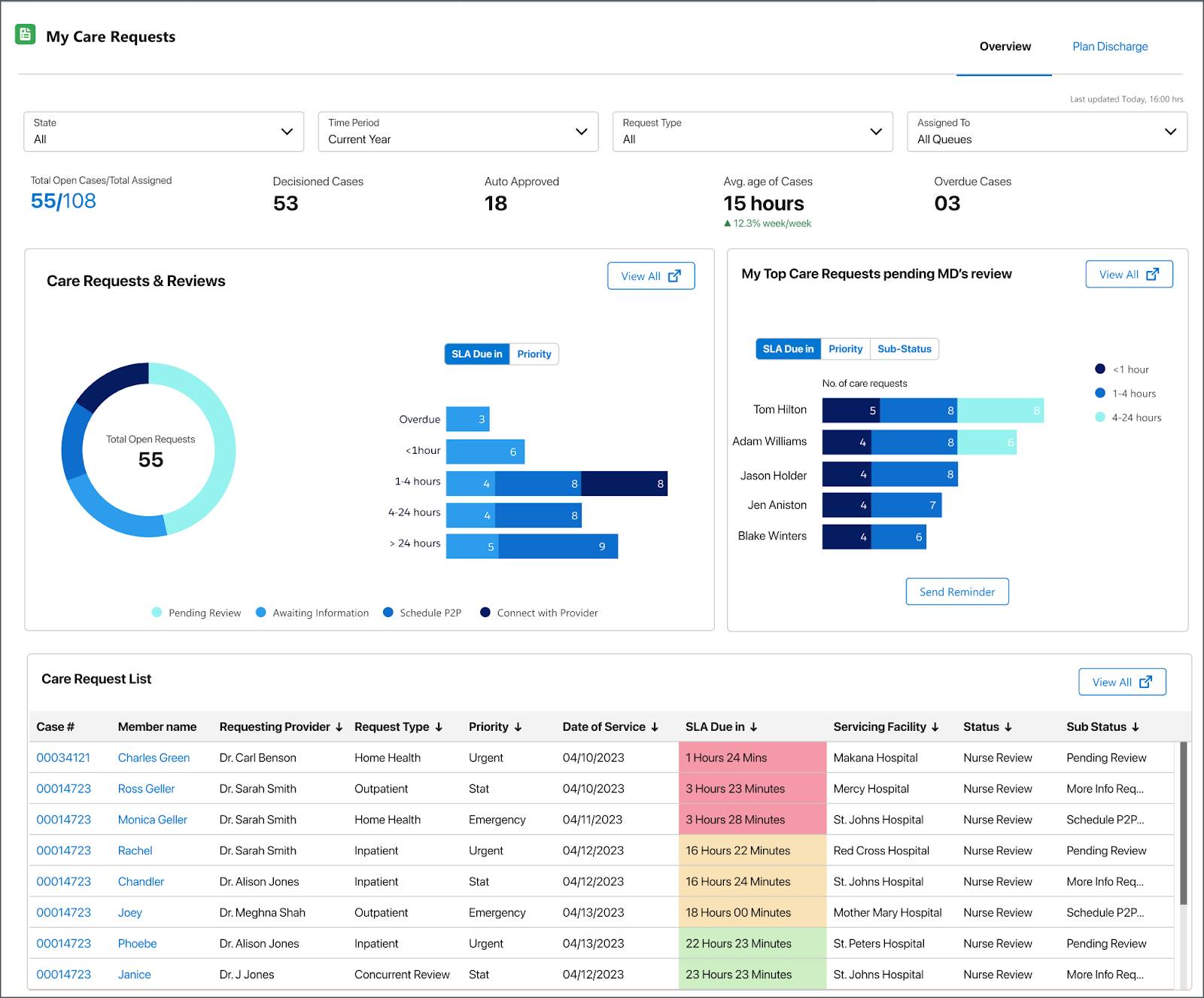
The UM Nurse guided flow empowers UM nurses to make informed decisions on requested services. Using the flow, the nurses can refer the case to the medical director (MD) for review, and request additional information from the provider when needed.
Decision and Communication
Medical directors struggle to quickly access patient clinical information to conduct their reviews. When they do come to a determination, medical directors don’t have a simple way to communicate a complete summary and recommendation.
The integrated platform offers a comprehensive 360-degree view for quick review and determination. The UM nurse can easily hand off any PA review to the medical director, with all recommendations and other key information consolidated in one central location.
The medical director workflow gives a holistic view of the entire authorization process, with pre-configured components for member and provider details. The workflow also provides the directors with the ability to add contextual notes against requested services and other documents.
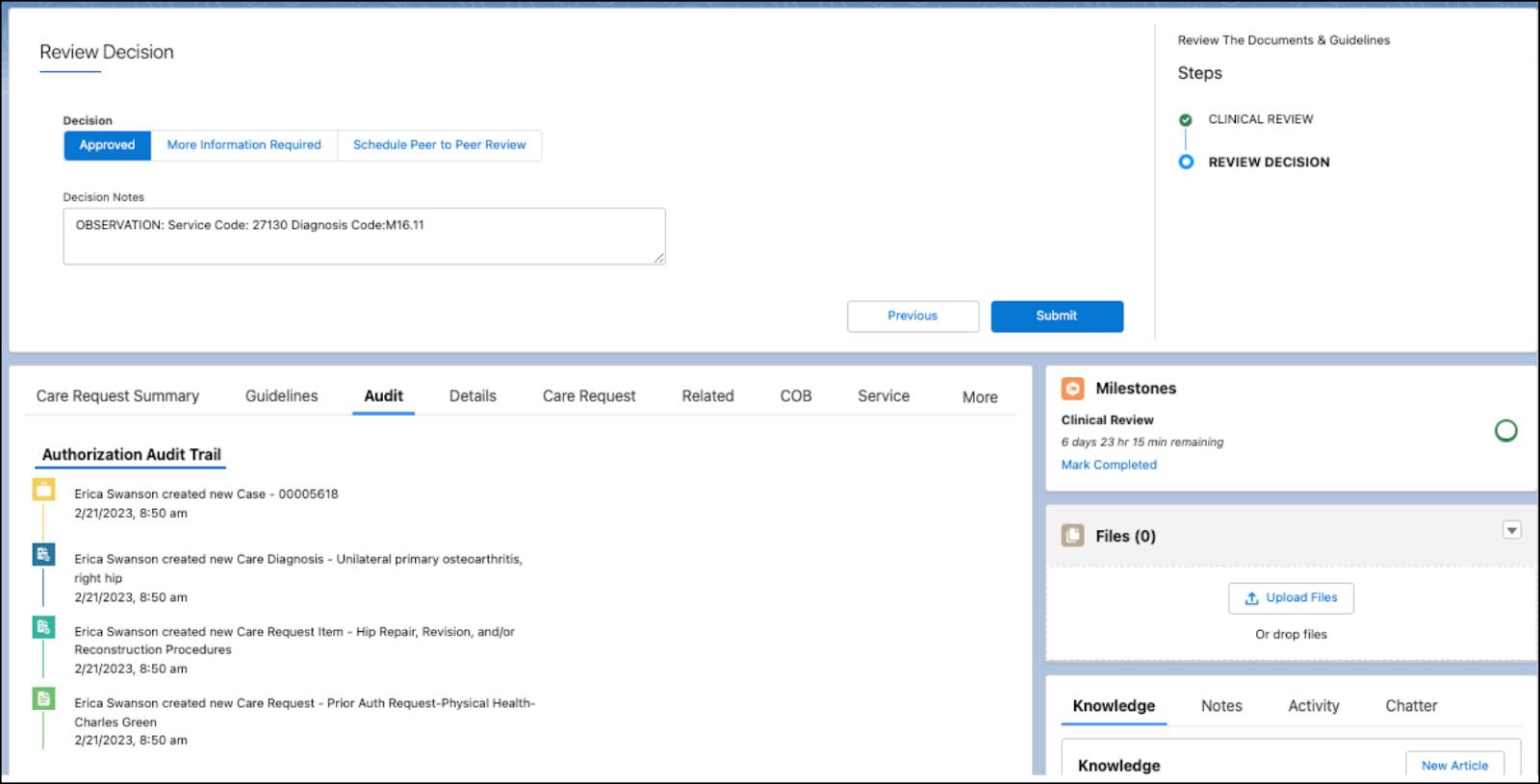
For peer-to-peer (P2P) review, UM nurses can schedule a review and record any interaction notes. Using Lightning Scheduler, nurses can view the MD availability based on Lightning Scheduler resource setup. And when it's time for their scheduled review, the MD can record information about the interaction in the same view.
Additional Tools
All of these features are only a small sample of the Health Cloud tools that empower users to build more efficient and effective utilization management processes.
To help analyze and optimize UM operations, CRM Analytics for Healthcare is available as an add-on product. It includes UM analytics and AI capabilities, which give organizations actionable data and insight across the UM lifecycle.
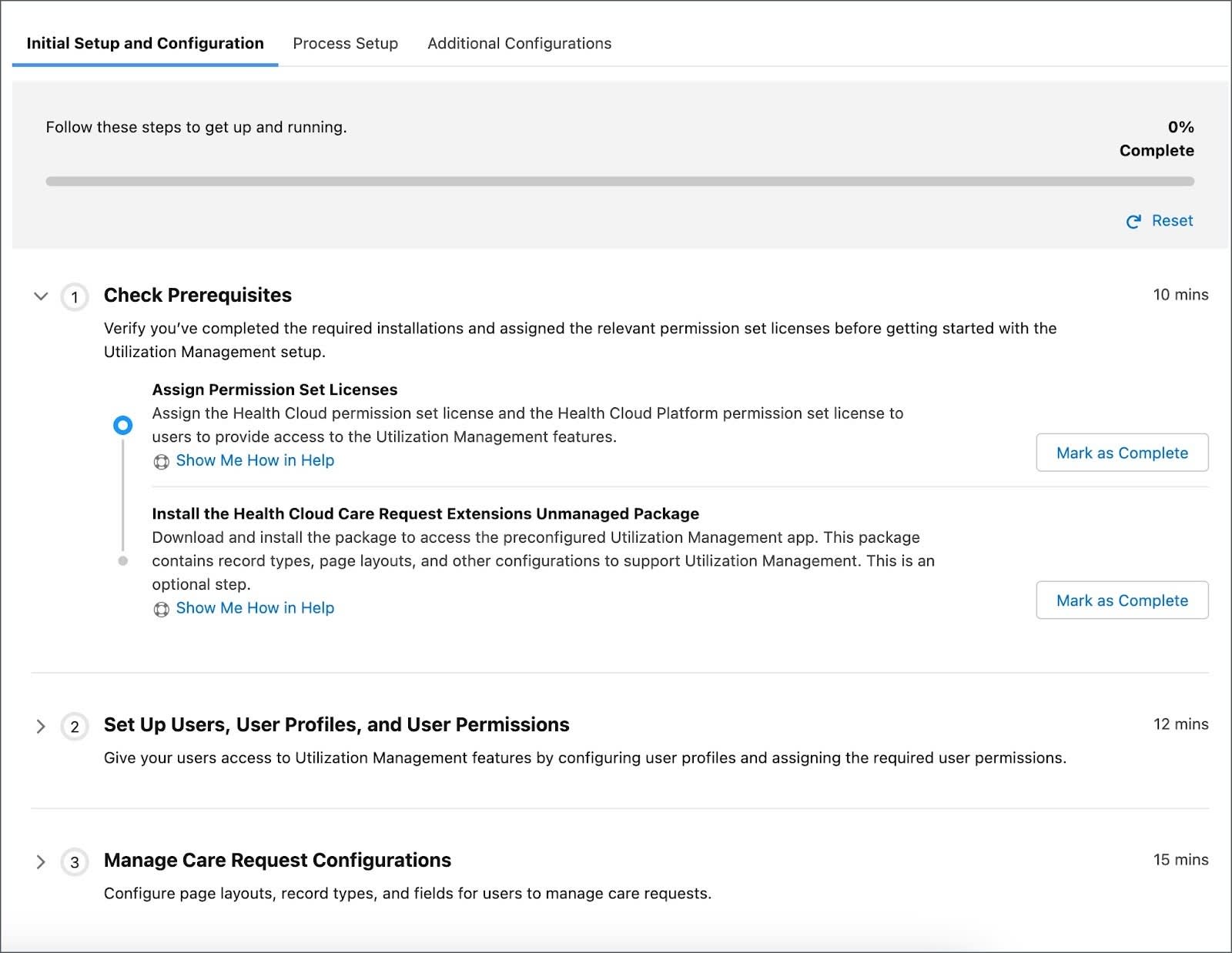
To assist users in quickly configuring all of these powerful features, Health Cloud provides Salesforce Easy, a guided workflow that offers a unified view of all key setup steps. It keeps track of all the stages and enables users to pick up where they left off.
As you can see, Health Cloud equips users with a comprehensive toolkit to build efficient, data-driven utilization management processes.
A Unified Solution
Ultimately, UM offers substantial benefits for payers, providers, and members alike. For payers, it ensures cost-effective healthcare by reviewing and approving appropriate treatments and services, and minimizing unnecessary expenses. Providers benefit from UM through streamlined workflows, improved coordination of care, and enhanced communication with payers. This results in optimized resource allocation and increased efficiency. Meanwhile, members benefit from this process as it helps ensure they receive the right care at the right time, promoting patient safety, reducing treatment delays, and enhancing overall healthcare outcomes.
Health Cloud not only simplifies and optimizes the coordination across various stakeholders, it also integrates utilization management, care management, and customer service processes into a single solution.
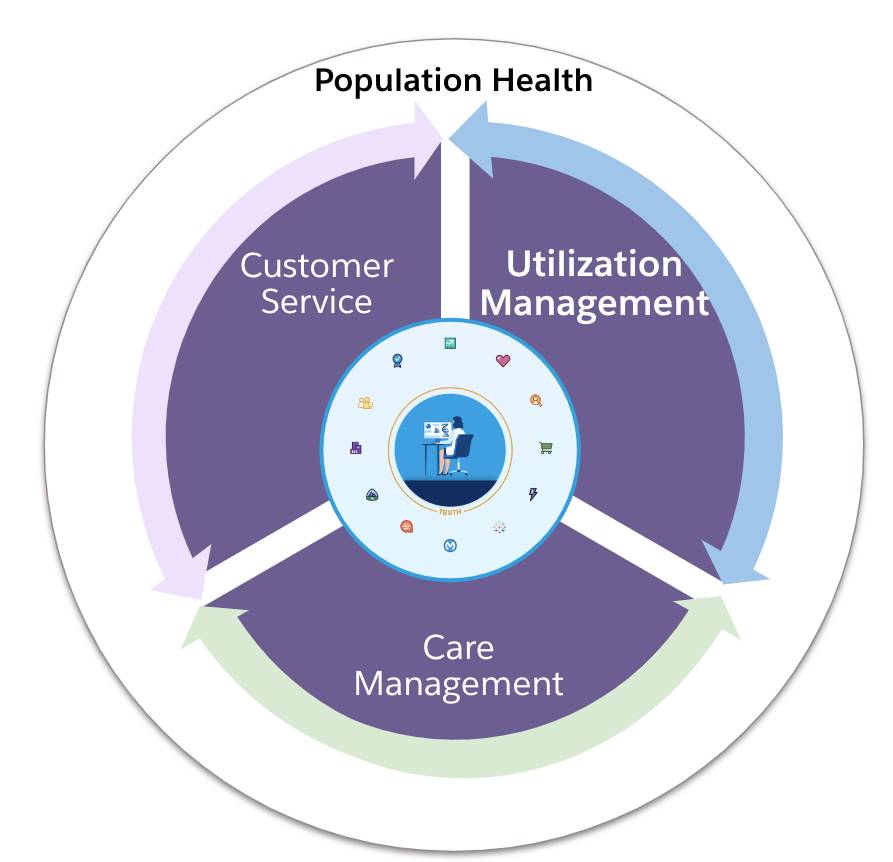
The PA intake begins with provider customer service workflows that initiate clinical utilization management processes. And PA requests can then trigger program enrollment in care management programs. The care management solution can monitor for discharge planning opportunities from UM and review updates to cases on currently engaged members. All of these solutions work together to form a unified ecosystem.
Seamlessly bringing all these complex processes into a single platform helps health organizations lower operational costs and, most importantly, improve patient health and member satisfaction.
In this unit, you learned how Utilization Management provides a variety of features and workflows for helping providers and payers navigate the entire UM lifecycle. In the next unit, explore how Health Cloud empowers providers to submit authorization requests with ease.
Resources
- Trailhead: Health Cloud Data Models for Healthcare
- Trailhead: OmniScripts
- Trailhead: Intelligent Document Automation for Health Cloud
- Trailhead: Business Rules Engine
- Salesforce Help: Handle Care Requests with Utilization Management